Alcohol-Opioid Risk Calculator
Alcohol & Opioid Risk Calculator
Enter your opioid dose and blood alcohol concentration to see how much your breathing is suppressed. No safe level exists - this is a simulation.
Your Breathing Suppression Risk
Call 911 immediately
Why This Matters
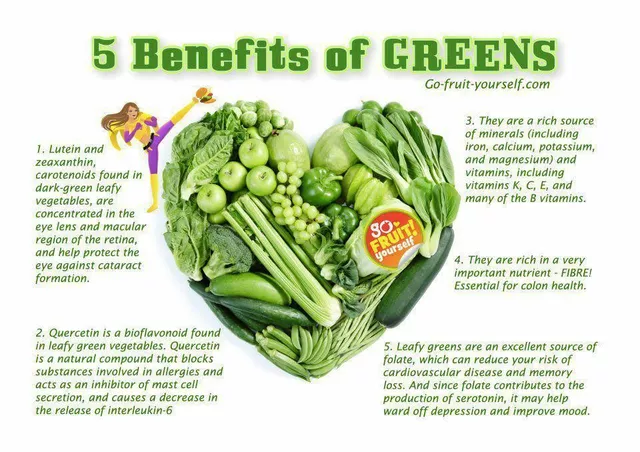
Article Fact: 20mg oxycodone alone reduces breathing by 28%. Add alcohol at legal limit (0.08 BAC) and breathing drops another 19%.
Important Note: This calculation shows only the respiratory suppression risk. Actual overdose can occur at any combination due to individual factors.
When you mix alcohol and opioids, you’re not just adding two substances together-you’re creating a dangerous chemical storm inside your body. The risk isn’t just higher. It’s exponentially deadlier. This isn’t theoretical. It’s happening right now, in homes, hospitals, and emergency rooms across the U.S., including right here in Pittsburgh. Every year, thousands of people die from this exact combination. And many of them never meant to overdose.
Why This Combination Is So Deadly
Both alcohol and opioids slow down your central nervous system. That’s why opioids are used for pain relief and alcohol makes you feel relaxed. But when they’re together, they don’t just add up-they multiply. Your breathing slows. Then it gets uneven. Then it stops. That’s how overdose kills: not from heart failure, not from liver damage, but from simply forgetting how to breathe. A 2017 study showed that 20mg of oxycodone alone reduced breathing by 28%. Add just enough alcohol to hit the legal driving limit-0.1% blood alcohol concentration-and breathing dropped another 19%. That’s not a small increase. That’s a near-total collapse of your body’s ability to stay alive. Older adults, people with existing lung conditions, or those taking higher doses of opioids are at even greater risk. The FDA issued a black-box warning in 2016-the strongest possible alert-for all prescription opioids. The message was clear: alcohol and opioids together can kill you. This wasn’t based on guesswork. It came from years of toxicology reports, emergency room data, and autopsy findings. In 2022 alone, 107,941 drug overdose deaths occurred in the U.S. Eighty-one percent of those involved multiple substances. Alcohol was in the mix more often than most people realize.Which Opioids Are Most Dangerous with Alcohol?
Not all opioids carry the same risk, but the ones most commonly prescribed are the most dangerous when mixed with alcohol. Hydrocodone (Vicodin), oxycodone (OxyContin), and fentanyl are the top culprits. Fentanyl is especially terrifying because it’s 50 to 100 times stronger than morphine. Even a tiny amount can stop breathing-and alcohol makes that threshold even lower. Data from Texas shows that between 2010 and 2019, alcohol was involved in 37% of all polysubstance deaths involving alcohol and another drug. Of those, 77% were men. But the trend isn’t just about gender-it’s about access and misunderstanding. Many people think, “I’m only having one drink,” or “I took my pain pill last night, so it’s out of my system.” Neither is true. Prescription opioids still account for a large share of these deaths. In 2019, alcohol was found in 15% of opioid-related deaths, up from 12% in 2010. Synthetic opioids like fentanyl saw the steepest rise-alcohol co-involvement jumped from 9% to 17% in that same period. That means more people are combining street drugs with alcohol, often without knowing what they’re actually taking.What Happens in Your Body When You Mix Them?
Your brain has a control center for breathing. Opioids bind to receptors there and turn down the signal. Alcohol does the same thing-just through different pathways. When both are present, they overwhelm the system. Your brain stops telling your lungs to inhale. Your oxygen levels drop. Your heart struggles. You lose consciousness. And because both substances dull your awareness, you won’t feel the warning signs until it’s too late. Post-mortem studies show something even more chilling: alcohol lowers the amount of opioid needed to cause death. In cases involving buprenorphine-a medication used to treat opioid addiction-30% of fatal overdoses also had alcohol in the system. That means someone taking a prescribed, supposedly safe dose of buprenorphine could die if they had even one glass of wine. Methadone patients are especially vulnerable. Research found they were 4.6 times more likely to die from overdose if they drank alcohol. That’s not a small risk. That’s a life-or-death red flag.
Who’s at Risk-and Why They Don’t Realize It
People who take opioids for chronic pain are often told to avoid alcohol. But many don’t think it applies to them. “I’m not addicted,” they say. “I just take it for my back.” They might have a drink at dinner. Or take a pain pill after a long day and a beer. It feels harmless. Others are using opioids recreationally, or they’re using street drugs like heroin or counterfeit pills laced with fentanyl. They don’t know what’s in the pill. They don’t know how strong it is. And they don’t realize alcohol makes it even more unpredictable. People with alcohol use disorder are 3.2 times more likely to overdose on opioids, according to the American Society of Addiction Medicine. That’s not a coincidence. It’s a pattern. The same brain pathways that drive addiction to one substance often overlap with the other. Treating one without addressing the other rarely works.What’s Being Done-and Why It’s Not Enough
There are warnings on pill bottles. There are FDA mandates. There are public health campaigns like SAMHSA’s “Don’t Mix” initiative, launched in January 2023 with $15 million to raise awareness. Hospitals are training staff to screen for alcohol use before prescribing opioids. Naloxone, the overdose reversal drug, is now more widely available. But here’s the problem: most people who die from this combination aren’t in treatment. They’re not in rehab. They’re not seeing a doctor. They’re at home. They’re alone. They’re not thinking about risk. They’re thinking about relief-from pain, from anxiety, from numbness. A 2023 study from the University of Pittsburgh found a potential early warning sign: reduced heart rate variability. In lab tests, this change predicted 83% of alcohol-opioid overdoses up to 30 minutes before breathing stopped. That’s promising for future monitoring devices-but it’s not helping anyone today. The CDC projects alcohol-opioid deaths will rise 7.2% each year through 2025 unless something changes. That’s not a trend. That’s a countdown.







Peter Sharplin January 25, 2026
Been working ER in Pittsburgh for 12 years. Saw this play out too many times. Guy takes his oxycodone for his back, has one beer after work, falls asleep, never wakes up. Family finds him at 7 a.m. with an empty bottle and a half-empty pill bottle. No drama. No warning. Just silent. The data in this post? Real. Every number is a person who thought they were being careful.
And yeah, the FDA warning’s on the bottle. But people don’t read it. Or they read it and think, ‘That’s for addicts.’ Wrong. It’s for everyone.
I’ve handed out naloxone kits to grandmas who take hydrocodone for arthritis. Told them: ‘If your grandkid comes over and you have a glass of wine, keep that kit by the bed.’ They laughed. Then their husband OD’d last winter. They still cry when they talk about it.
This isn’t about stigma. It’s about biology. Your brain doesn’t care if you’re ‘responsible.’ It just knows two depressants are on board. And it shuts down. No second chances.
Uche Okoro January 26, 2026
From a pharmacokinetic standpoint, the synergistic potentiation of CNS depression via GABAergic and mu-opioid receptor co-activation creates a non-linear dose-response curve where therapeutic indices collapse catastrophically. The hepatic metabolism of both substances-particularly CYP3A4-mediated oxidation of opioids and alcohol’s competitive inhibition of oxidative pathways-leads to prolonged half-lives and unpredictable serum concentrations.
Moreover, ethanol-induced gastric mucosal irritation exacerbates opioid absorption kinetics, increasing bioavailability. This is not merely additive-it’s multiplicative. The 19% additional respiratory depression at 0.1% BAC isn’t statistical noise-it’s a physiological cliff edge.
And the data on fentanyl co-ingestion? That’s a public health exothermic reaction. We’re not talking about recreational use anymore. We’re talking about accidental lethal pharmacodynamics in a polypharmacy-saturated environment.
Public health messaging fails because it’s emotional, not mechanistic. People need to understand the *why*, not just the ‘don’t.’
Josh josh January 26, 2026
dude i took a percocet after a beer once and just passed out for 3 hours no big deal lmao
Ryan W January 27, 2026
So let me get this straight-we’re banning alcohol because some dumbass can’t follow a warning label? This is why America’s falling apart. You want to save lives? Teach people to be responsible. Not treat adults like toddlers who can’t handle a glass of wine with their pain meds.
Meanwhile, China’s cranking out fentanyl pills and we’re busy scolding grandmas for having a glass of chardonnay. Pathetic.
Allie Lehto January 29, 2026
i just feel like if you’re taking opioids you’re already kinda asking for trouble?? like why even have the pain if you’re gonna numb it with chemicals??
also i think god sends signs when you do stuff like this… like my cousin’s friend’s sister died like this and she was always so full of light before…
also i think we need more prayer circles at the ERs
shivam utkresth January 30, 2026
Man, I grew up in Delhi where people mix painkillers with whiskey like it’s chai. No one talks about it. No one thinks it’s dangerous. My uncle took tramadol after a few pegs for his knee and woke up with his lungs on vacation. He survived, barely.
But here’s the thing-it’s not just about the science. It’s about culture. In India, pain is something you endure silently. You don’t go to the doctor. You don’t ask questions. You just pop something and drink something else to make it feel less real.
This post? It’s a mirror. And most of us are looking away.
Also, the part about buprenorphine and wine? That hit me. My cousin’s on Suboxone. I never told him I drink. Now I won’t. Ever.
SWAPNIL SIDAM January 31, 2026
Bro. One drink. Just one. You think you’re safe? You’re not. I saw a guy at my cousin’s wedding. Took his pain pill. Had one beer. Sat down. Never got up. No drama. No screaming. Just… gone.
My aunt cried for three months. She said, ‘He was just trying to enjoy the day.’
Don’t be that guy. Don’t be that family. One drink is all it takes. No second chances.
Mohammed Rizvi January 31, 2026
So let me get this straight: the government’s got a black-box warning, a $15M campaign, and still people are dying because they thought ‘one beer’ wouldn’t hurt?
Meanwhile, the same people who’d never mix drugs with alcohol? They’ll binge on opioids like it’s candy and then blame the system.
It’s not the pills. It’s the mindset. You don’t get to be ‘responsible’ while pretending you’re invincible.
And for the love of god, stop pretending you’re not part of the problem because you ‘only take it for back pain.’ You’re not a patient. You’re a statistic in the making.
Shawn Raja January 31, 2026
There’s a deeper truth here: we don’t mix alcohol and opioids because we’re stupid. We mix them because we’re exhausted.
People aren’t dying because they’re addicts. They’re dying because they’re tired. Tired of pain. Tired of anxiety. Tired of being told to ‘just push through.’
So they reach for the pill. And the drink. And the silence.
And when the system says ‘don’t mix,’ they hear ‘you’re not allowed to feel better.’
Maybe the real question isn’t how to stop the mixing.
It’s why they felt they had to mix in the first place.