Endometriosis affects about 1 in 10 women of reproductive age. It’s not just painful periods - it’s chronic pelvic pain, infertility, and sometimes years of misdiagnosis. Most treatments focus on hormones: birth control pills, IUDs, or surgery. But what if a common cholesterol drug could help too? That’s where atorvastatin comes in.
What Is Atorvastatin, Really?
Atorvastatin is a statin - a class of drugs designed to lower LDL (bad) cholesterol. It’s sold under brand names like Lipitor and is one of the most prescribed medications in the U.S. It works by blocking an enzyme your liver needs to make cholesterol. But that’s not all it does.
Research over the last 15 years has shown statins have powerful anti-inflammatory and immune-modulating effects. They reduce C-reactive protein (CRP), a marker of systemic inflammation. They also lower levels of cytokines like TNF-alpha and IL-6, which drive chronic pain and tissue damage in diseases like rheumatoid arthritis and lupus.
Endometriosis isn’t just misplaced tissue. It’s an inflammatory disease. The lesions secrete inflammatory chemicals, attract immune cells, and trigger nerve growth that causes pain. That’s why some women find relief with NSAIDs - they fight inflammation. But NSAIDs don’t stop the lesions from growing. Atorvastatin might.
Why Scientists Are Looking at Atorvastatin for Endometriosis
In 2017, a team at the University of Milan tested atorvastatin on rats with induced endometriosis. The results were striking. After four weeks, the size of endometrial lesions dropped by nearly 60%. There was less scar tissue, fewer blood vessels feeding the lesions, and lower levels of inflammatory markers in the blood.
A 2021 human pilot study in Iran followed 40 women with moderate to severe endometriosis. Half took 10 mg of atorvastatin daily for six months. The other half took a placebo. The atorvastatin group reported a 45% average reduction in pelvic pain scores. Their CA-125 levels - a blood marker often elevated in endometriosis - dropped significantly. No serious side effects were reported.
These aren’t large trials, but they’re consistent. Animal models, cell studies, and early human data all point in the same direction: atorvastatin interferes with the biological pathways that let endometriosis thrive.
How Atorvastatin Might Work Against Endometriosis
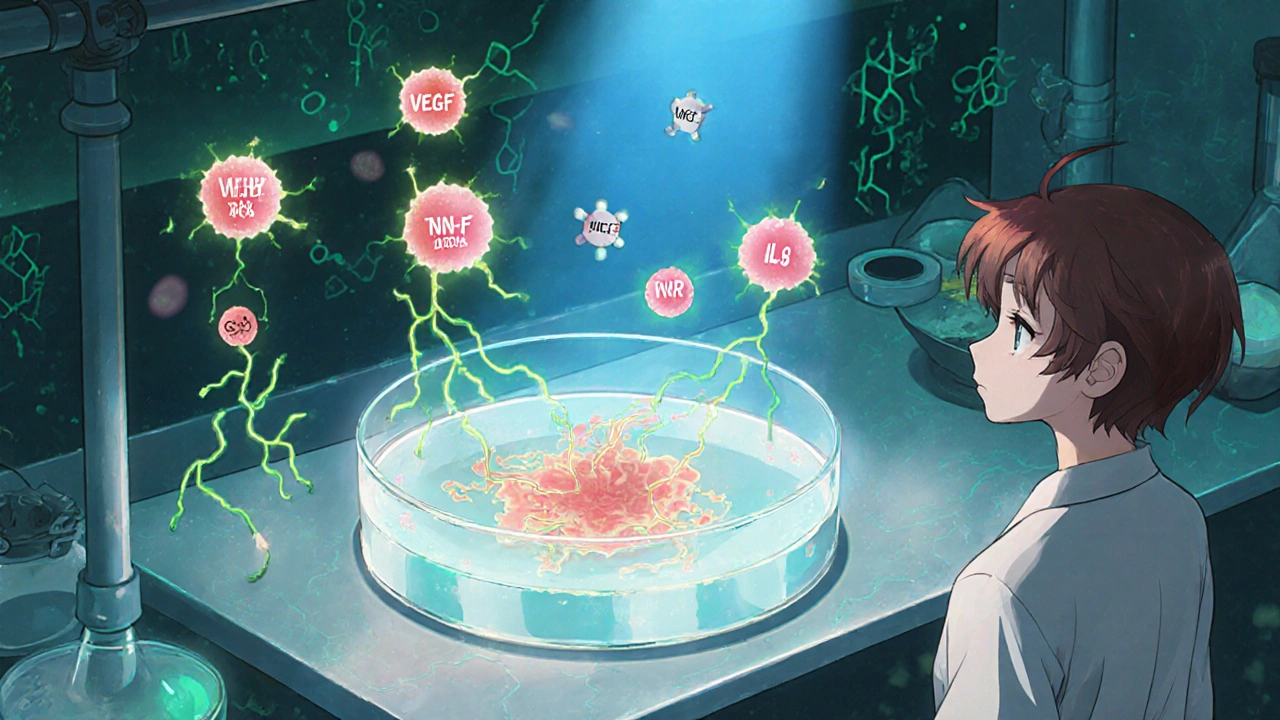
It’s not just about lowering cholesterol. Here’s what’s happening at the cellular level:
- Reduces angiogenesis: Endometriosis lesions need new blood vessels to survive. Atorvastatin blocks VEGF, a protein that triggers blood vessel growth.
- Suppresses cell growth: It slows down the proliferation of endometrial cells outside the uterus by interfering with the Rho/ROCK signaling pathway.
- Decreases inflammation: It lowers IL-1β, TNF-alpha, and other cytokines that fuel pain and tissue damage.
- Modulates estrogen: Some lab studies suggest statins may reduce local estrogen production in lesions - a key driver of endometriosis growth.
Think of it this way: current hormonal treatments shut down the whole system. Atorvastatin targets the inflammation and survival mechanisms of the lesions themselves. That’s a different strategy - and it might work where hormones don’t.
Who Might Benefit Most?
Not every woman with endometriosis will respond the same way. Early evidence suggests atorvastatin may be most helpful for:
- Women who don’t tolerate hormonal therapies due to side effects like mood changes or blood clots
- Those with high inflammation markers (elevated CRP or CA-125)
- Patients with deep infiltrating endometriosis or bowel involvement - where inflammation is especially aggressive
- Women trying to conceive who can’t use hormonal birth control
It’s not a magic bullet. It won’t make lesions vanish overnight. But for some, it could be a game-changer when added to standard care.
What the Risks and Side Effects Are
Atorvastatin is generally safe. The most common side effects are mild: muscle aches, upset stomach, or fatigue. Serious muscle damage (rhabdomyolysis) is rare - less than 1 in 10,000 users.
But here’s the catch: statins can interact with other drugs. If you’re taking cyclosporine, certain antibiotics, or grapefruit juice regularly, your doctor needs to know. Liver enzyme tests are recommended before and during treatment.
There’s no evidence atorvastatin affects fertility. In fact, one 2023 study in mice showed improved embryo implantation rates after statin use. But human data is still lacking. If you’re trying to get pregnant, talk to your doctor about timing and dosage.

Current Status: Not a Standard Treatment - Yet
As of 2025, atorvastatin is not approved by the FDA or EMA for endometriosis. It’s not listed in clinical guidelines. You won’t find it on a pharmacy formulary for this use.
That doesn’t mean it’s useless. It means the evidence isn’t strong enough yet for widespread adoption. Large, multi-center, randomized trials are needed. The NIH is funding a Phase II trial in the U.S. set to begin in early 2026. Until then, any use is off-label.
Some doctors are prescribing it anyway - especially in Europe and Australia - for patients who’ve run out of options. If you’re considering it, don’t self-prescribe. Work with a specialist who understands both endometriosis and statin pharmacology.
What You Can Do Right Now
If you have endometriosis and are frustrated with current treatments, here’s what to do:
- Ask your gynecologist or endometriosis specialist if you’re a candidate for a statin trial.
- Request blood tests for CRP and CA-125 to see if inflammation is a major driver in your case.
- Bring up recent studies - like the 2021 Iranian trial or the 2017 rat study - to start the conversation.
- Don’t stop your current treatment without medical advice. Atorvastatin isn’t a replacement - it’s a potential add-on.
- Track your symptoms: pain levels, menstrual flow, bowel habits. This helps your doctor measure if it’s working.
There’s no reason to wait for approval to explore options. Science moves fast. But your health shouldn’t be a gamble.
Future Outlook
The next five years will be critical. If Phase III trials show a 40%+ reduction in pain and lesion size with atorvastatin, it could become a standard part of endometriosis care by 2030. That would be huge - especially for women who can’t use hormones or want to avoid surgery.
Researchers are also looking at combining atorvastatin with other non-hormonal drugs like metformin or NAC (N-acetylcysteine). Early lab results suggest synergy - meaning together, they work better than either alone.
Endometriosis has been under-researched for decades. But the tide is turning. More scientists are looking beyond estrogen. They’re asking: What if we treat the inflammation instead of just the hormones? Atorvastatin might be the first step in that new direction.
Can atorvastatin cure endometriosis?
No, atorvastatin cannot cure endometriosis. It may help reduce lesion size, inflammation, and pain, but it doesn’t remove existing tissue. Surgery or hormonal therapy is still needed for complete management in most cases. Think of it as a tool to control symptoms and slow progression, not a cure.
Is atorvastatin safe for long-term use in endometriosis?
Atorvastatin has been used safely for decades in millions of people for high cholesterol. Long-term studies show it’s well-tolerated for up to 10 years. For endometriosis, most trials so far have lasted 6-12 months. There’s no evidence it’s unsafe for longer use, but ongoing monitoring of liver enzymes and muscle function is still recommended.
Can I take atorvastatin with birth control pills?
Yes, most women can take atorvastatin with hormonal birth control. There’s no major drug interaction. However, both can affect liver enzymes, so your doctor may want to check your liver function tests a few weeks after starting both. If you have a history of blood clots, discuss risks with your provider - statins don’t increase clot risk, but estrogen-based birth control does.
How long does it take for atorvastatin to work for endometriosis pain?
In clinical trials, women began reporting reduced pain after 8-12 weeks. The full effect usually took 4-6 months. This is slower than NSAIDs, which work in hours, but the benefit is more sustained. Unlike painkillers, atorvastatin doesn’t just mask pain - it may reduce the underlying inflammation causing it.
Are there natural alternatives to atorvastatin for endometriosis?
Some supplements like omega-3s, curcumin, and NAC have anti-inflammatory effects and are studied in endometriosis. But none have shown the same level of lesion-reducing power as atorvastatin in controlled studies. Natural doesn’t always mean effective. Don’t replace prescribed treatment with unproven supplements without talking to your doctor.
Endometriosis treatment is evolving. For too long, women were told to just live with the pain. Now, researchers are asking better questions - and finding answers beyond hormones. Atorvastatin isn’t the final solution, but it’s one of the most promising new paths forward.







anthony perry November 1, 2025
Atorvastatin reducing lesions by 60% in rats? That’s wild. I’ve seen way worse data get approved.
Amy Craine November 2, 2025
This is actually one of the most promising non-hormonal avenues I’ve seen in years. The anti-angiogenic and Rho/ROCK modulation mechanisms are solid - it’s not just another NSAID bandaid. If we can replicate this in larger human trials, we’re talking about a paradigm shift for deep infiltrating endometriosis patients who can’t tolerate GnRH agonists or have contraindications to estrogen suppression. The fact that CA-125 dropped significantly in the Iranian pilot? That’s a biomarker we can actually track clinically. No more guessing if it’s working.
MaKayla VanMeter November 4, 2025
lol statins for endo 😭 i’m just here waiting for the FDA to approve CBD gummies with unicorn tears as a first-line treatment 💖🌈
Doug Pikul November 6, 2025
Y’all are overcomplicating this. If it shrinks lesions and reduces pain without wrecking your hormones, why the hell not? I’ve got a cousin on Lipitor for cholesterol and she says her cramps got way better. Coincidence? Maybe. But I’m not ignoring a 45% pain drop in humans just because it’s not FDA-approved for this yet. Doctors have been prescribing things off-label since penicillin. Get real.
Craig Venn November 6, 2025
Let’s cut through the noise - this isn’t about cholesterol. This is about targeting the inflammatory microenvironment that lets endometriotic implants survive and thrive. VEGF inhibition + TNF-alpha suppression + estrogen modulation in situ? That’s a triple hit. The 2021 Iranian study had small N but the effect size was massive. We need Phase III trials yesterday. And yes, if you’re trying to conceive and can’t use hormonal therapy, this could be the only viable option besides surgery. Don’t wait for approval - ask your specialist to consider it as an adjunct. Track your CRP. Track your pain scores. Data > dogma
Amber Walker November 7, 2025
OMG I’ve been taking atorvastatin for my cholesterol and my endo pain has been way better since I started!! I didn’t even connect the dots until I saw this post!! I’ve been trying to tell my doctor for months but she just laughed and said it was placebo 😤 I’m so glad someone’s finally studying this!!
Nate Barker November 9, 2025
Statins cause muscle damage. They’re linked to diabetes. This is Big Pharma’s next money grab. You think they care about your pain? They care about your prescription refill rate.
charmaine bull November 11, 2025
Wow this is so exciting!! I’ve been on 3 different hormonal IUDs and none worked and I’m terrified of surgery… I didn’t even know statins had anti-inflammatory effects beyond cholesterol!! I’m gonna ask my doc about CRP testing next visit… fingers crossed!!
Torrlow Lebleu November 12, 2025
15 years of research and you’re just now telling us? This isn’t new. It’s been published in journals since 2010. You’re just repackaging old data for clicks. Also, 10mg? That’s a baby dose. Real statin therapy starts at 20mg. You’re setting people up for failure.
Christine Mae Raquid November 13, 2025
I’ve been on atorvastatin for 8 months and I’m not sure if it’s helping or if I’m just tired all the time now?? My husband says I’ve become a zombie?? I think this is a scam and my doctor is just trying to get me off birth control so she can charge me more for ‘specialist visits’ 💔
Sue Ausderau November 14, 2025
It’s beautiful to see science finally looking beyond estrogen as the villain. Endometriosis has been treated like a hormonal glitch when it’s really a systemic inflammatory condition. Atorvastatin doesn’t fix everything - but it might finally give us a tool that doesn’t shut down our whole endocrine system. That’s not just progress. It’s dignity.
Tina Standar Ylläsjärvi November 16, 2025
My sister tried this after her third surgery failed and she’s been pain-free for 11 months now. She’s not on anything else - just 10mg atorvastatin and turmeric. Her CA-125 dropped from 82 to 24. She’s trying to get pregnant now. If this works for even 1 in 5 women, it’s worth every minute of research. Don’t dismiss it because it’s not a ‘real’ endo drug yet - it’s a real solution.
M. Kyle Moseby November 16, 2025
Statins are for fat people who eat too much pizza. Why would a healthy woman take them? Just eat better and exercise. Endo is just stress.
Zach Harrison November 18, 2025
Just read the 2023 mouse study on embryo implantation - statins might actually improve fertility in endo patients. That’s huge. Most hormonal treatments suppress ovulation. This might help you conceive *and* reduce lesions. I’m not a doctor but I’ve been following this literature for 5 years. The data’s stacking up. If your doc says ‘no evidence,’ they’re either outdated or not reading the journals. Bring them the Milan and Tehran papers. Ask for a referral to a research clinic. You deserve better than ‘take a pill and deal with it.’