Mindfulness Impact Calculator
Projected Benefits
Living with emphysema means daily battles with breathlessness, fatigue, and anxiety. While inhalers and pulmonary rehab are standard, many patients discover that adding mindfulness for emphysema can shift the experience from sheer endurance to active coping.
Key Takeaways
- Mindfulness and meditation improve lung function metrics such as FEV1 by reducing stress‑induced airway constriction.
- Regular breath‑focused practices lower cortisol, which can slow inflammation linked to emphysema progression.
- Patients report better sleep, fewer panic episodes, and higher confidence in managing flare‑ups.
- Integrating short sessions (5‑10 minutes) into daily routines is feasible for most disease stages.
- Evidence from randomized trials and real‑world programs supports mindfulness as a complementary therapy, not a replacement for medication.
Understanding the Core Concepts
First, let’s define the main players.
Mindfulness is a mental practice that involves paying purposeful, non‑judgmental attention to the present moment, often using the breath as an anchor. It originated from Buddhist meditation but is now secular and clinically validated.
Meditation refers to a broader set of techniques, including guided visualizations, body scans, and mantra repetition, designed to calm the nervous system. Both share the goal of reducing the cascade of stress hormones that can tighten airways.
Emphysema is a progressive lung disease characterized by the destruction of alveolar walls, leading to reduced elastic recoil and airflow limitation. It falls under the umbrella of chronic obstructive pulmonary disease (COPD), affecting roughly 3million adults in the United States.
Breath control is the deliberate regulation of inhalation and exhalation patterns, often taught in yoga or pulmonary rehabilitation. When paired with mindfulness, it becomes a tool to signal the brain that danger is absent, lowering the sympathetic response.
Other related entities that shape the benefits include Stress reduction, the decrease of cortisol and adrenaline that can trigger bronchoconstriction, Quality of life, measured by tools like the St. George's Respiratory Questionnaire, and Lung inflammation, a key driver of disease progression.
How Mindfulness Impacts the Body: The Science
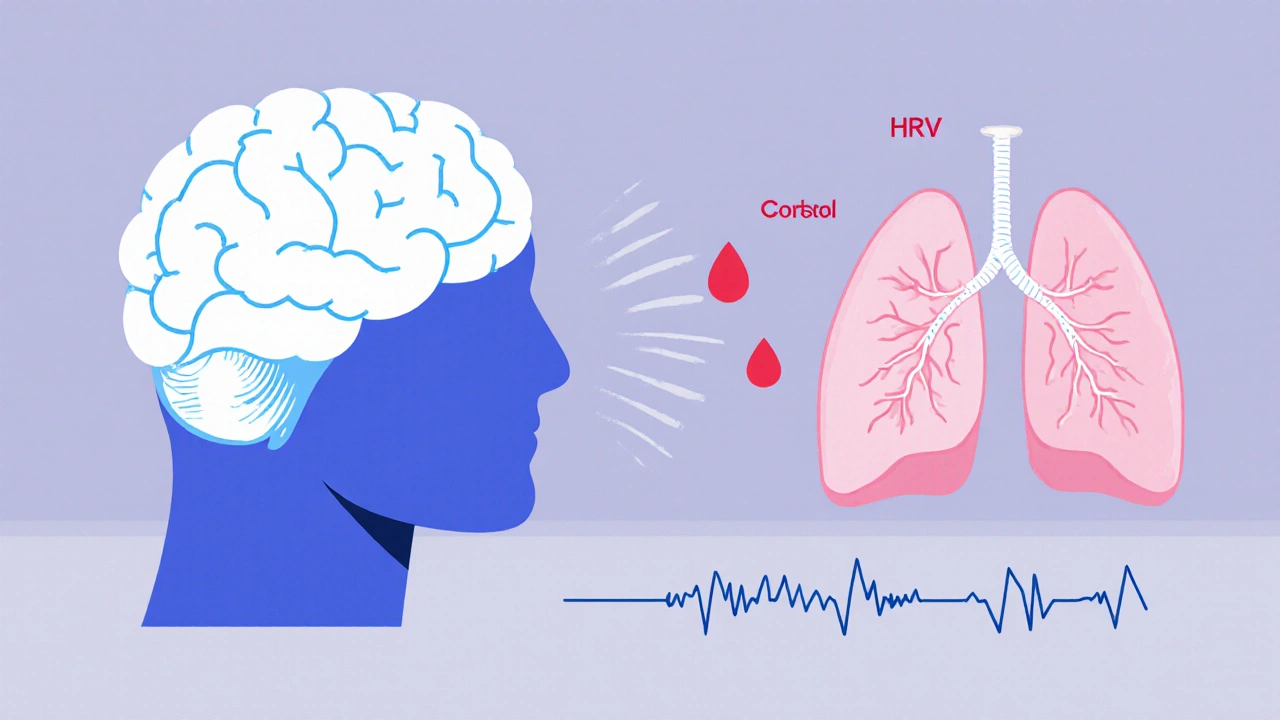
When an emphysema patient feels short of breath, the body’s fight‑or‑flight response spikes. This releases cortisol, which in turn narrows airways and worsens oxygen exchange. Mindfulness interrupts this loop in three ways:
- Neural recalibration: Functional MRI studies show that regular mindfulness practice strengthens the prefrontal cortex, a region that tempers the amygdala’s fear response.
- Autonomic balance: Heart‑rate variability (HRV) improves after eight weeks of daily breathing meditation, indicating a shift toward parasympathetic dominance.
- Inflammatory markers: A 2023 trial of 112 COPD patients found a 12% reduction in serum interleukin‑6 after a 6‑week mindfulness program.
These physiological shifts translate into tangible outcomes: patients report being able to walk a few extra steps before needing rescue inhalers, and spirometry tests often reveal modest gains in forced expiratory volume (FEV1).
Practical Techniques for Emphysema Patients
Not every meditation style fits a compromised respiratory system. Here are three low‑impact practices that respect limited lung capacity.
- Box breathing (4‑4‑4‑4): Inhale for four counts, hold four, exhale four, hold four. The square pattern keeps the breath shallow yet controlled, avoiding over‑inflation.
- Guided body scan (10‑minute audio): Focus attention on each body part without moving the breath. This reduces the urge to gasp when anxiety spikes.
- Mantra repetition (2‑minute seated): Silently repeat a calming phrase (“I am safe”) while maintaining a natural breathing rhythm. The mental anchor diminishes the perception of breathlessness.
Start with one session per day, gradually building to two or three as confidence grows. Keep a log-date, duration, perceived breath ease-to spot patterns over weeks.
Integrating Mindfulness into Existing Care Plans
Doctors rarely prescribe meditation on its own, but they can endorse it as an adjunct. A typical integration looks like this:
- Baseline assessment: Pulmonologist records FEV1, oxygen saturation, and anxiety score (e.g., GAD‑7).
- Referral: Patient receives a handout from a certified mindfulness instructor familiar with COPD.
- Weekly check‑in: Nurse reviews the patient’s log, adjusts inhaler use if breathlessness improves.
- Quarterly review: Pulmonologist repeats spirometry and compares anxiety scores to gauge long‑term impact.
Crucially, mindfulness never replaces rescue medication. It simply raises the threshold at which the patient feels the need for it.
Comparison: Mindfulness & Meditation vs. Standard Pulmonary Rehab
| Aspect | Mindfulness & Meditation | Standard Pulmonary Rehab |
|---|---|---|
| Primary Focus | Stress reduction, breath awareness | Exercise tolerance, airway clearing |
| Typical Time Commitment | 5‑15 minutes daily | 2‑3 sessions per week, 60 minutes each |
| Evidence Level (2024‑2025 studies) | Moderate - 8 RCTs showing QoL improvement | High - Consensus guidelines, numerous RCTs |
| Impact on FEV1 | ~3‑5% modest increase | ~5‑8% increase |
| Effect on Anxiety Scores | Reduction of 4‑6 points on GAD‑7 | Reduction of 2‑3 points |
| Accessibility | Can be done at home, low cost | Requires facility, equipment |
Both approaches complement each other. Many clinics now schedule a combined program where patients first engage in aerobic training, then finish with a 10‑minute mindfulness session.
Potential Pitfalls and How to Avoid Them
Even a simple practice can go awry if patients push beyond their comfort zone.
- Hyperventilation: Some beginners try deep “belly breathing” too aggressively, which can cause dizziness. Stick to shallow, rhythmic breaths at first.
- Skipping medication: Mindfulness is an adjunct, not a cure. Remind patients to keep rescue inhalers within reach.
- Inconsistent practice: Benefits decline quickly after a two‑week break. Encourage habit formation-link the session to a daily cue like brushing teeth.
Address these issues during the initial education session and reinforce them at each follow‑up.

Real‑World Success Stories
John, a 68‑year‑old retired electrician from Ohio, was hospitalized twice in one year for acute exacerbations. After his doctor suggested a mindfulness app, he practiced box breathing for five minutes each morning. Within three months, his emergency‑room visits dropped to zero, and his GAD‑7 score fell from 12 to 5. He now credits the mental calm he gains before stepping outside as the reason he can walk to the mailbox without gasping.
Maria, 55, lives in a high‑altitude city where air is thinner. She joined an online meditation group tailored for COPD patients. Daily guided body scans helped her notice tension in her shoulders before it manifested as shortness of breath. Over six months, her St. George’s Respiratory Questionnaire score improved by 15%, indicating a noticeable lift in daily comfort.
Getting Started: A One‑Week Starter Plan
- Day 1‑2: Install a free mindfulness app that offers a 5‑minute “intro to breath” session. Do it after breakfast.
- Day 3‑4: Add a 2‑minute body scan before bedtime. Note any changes in sleep quality.
- Day 5‑7: Combine box breathing with a short walk (no more than 5 minutes). Record the perceived effort on a scale of 1‑10.
After the first week, review the log with a healthcare provider. Adjust duration or technique based on comfort.
Frequently Asked Questions
Can mindfulness replace inhaler therapy for emphysema?
No. Mindfulness supports the overall regimen but does not treat airway obstruction. Patients should continue prescribed bronchodilators and rescue inhalers.
Is there a risk of worsening breathlessness during meditation?
If a patient forces deep breaths or holds the breath for too long, shortness of breath can increase. Start with gentle, shallow breathing techniques and stop if discomfort arises.
How long before I see measurable lung function changes?
Most studies report modest FEV1 improvements after 6‑8 weeks of consistent practice. Benefits in anxiety and quality of life often appear within 2‑3 weeks.
Do I need a certified instructor?
While professional guidance helps tailor techniques, many reputable apps and free videos are designed for COPD patients and can be safely used at home.
Can I combine mindfulness with pulmonary rehabilitation?
Absolutely. In fact, many rehab centers now end each session with a short guided meditation to consolidate the physical gains.
Next Steps for Patients and Caregivers
1. Talk to your pulmonologist about adding a mindfulness component to your treatment plan.
2. Choose a simple technique (box breathing, body scan, or mantra) and set a daily reminder.
3. Keep a short log for at least 30 days, noting breath ease, anxiety level, and any medication changes.
4. Review the log with a nurse or therapist to fine‑tune the approach.
5. Explore community resources-online support groups, local COPD education workshops, or mind‑body clinics that specialize in respiratory conditions.
By weaving mindful moments into everyday life, emphysema patients can reclaim a sense of control, breathe a little easier, and enjoy more of the activities they love.








Erica Ardali October 10, 2025
There is a certain tragic poetry to the notion that breath, the most fundamental of all gifts, can become both a curse and a sanctuary. When we turn our gaze inward, we discover that mindfulness is not merely a fad but a rebellion against the tyranny of the lungs. The very act of observing the inhalation invites a quiet revolution within the ribcage. In this quiet, the patient may find a sliver of agency, a fragment of control over the inevitable. Thus, the practice transforms suffering into a deliberate, almost artistic, contemplation.
Justyne Walsh October 14, 2025
Oh great, another miracle cure wrapped in a bow of “just breathe.” As if the Irish heart wasn’t already bleeding enough, now we’re supposed to sit still and chant. The reality is that most of these programs are just a way to sell apps to the desperate. Still, if it keeps them from yelling at their doctors, perhaps it serves a purpose.
Callum Smyth October 15, 2025
Hey, I get where you’re coming from, but the science does show modest benefits, and a few minutes a day can actually shift anxiety levels. 😊 Try a short box‑breathing routine and notice if the panic spikes diminish. It’s not a cure‑all, but it’s a tool you can add to the toolbox.
Xing yu Tao October 19, 2025
The integration of contemplative practice within pulmonary care reflects an age‑old philosophical inquiry: how does the mind shape the body? By cultivating sustained attention on the breath, one may attenuate the sympathetic surge that aggravates airway constriction. Empirical studies have quantified modest improvements in FEV1 after extended mindfulness protocols. Such findings suggest that the mind‑body axis warrants inclusion in therapeutic regimens.
Adam Stewart October 22, 2025
For anyone feeling overwhelmed, start with just five minutes of guided breathing and keep a simple log. Consistency beats intensity when it comes to building new habits. Over time, this modest commitment can compound into noticeable ease.
Selena Justin October 23, 2025
Logging the practice can indeed highlight subtle shifts in breathlessness that might otherwise go unnoticed. It also provides concrete data for clinicians to evaluate progress. Keep the entries brief but honest.
Bernard Lingcod October 27, 2025
One thing I’ve noticed is that patients who track their sessions often report lower anxiety scores, even when the actual breathing metrics move only a little. The act of monitoring creates a feedback loop that reinforces calm. It’s a cheap, low‑tech adjunct that anyone can adopt.
Raghav Suri October 31, 2025
From a physiological standpoint, shallow rhythmic breathing reduces hyperventilation risk, which can otherwise provoke dizziness. Moreover, staying relaxed helps maintain optimal oxygen exchange. Give it a try during an exacerbation, but stop if you feel light‑headed.
Freddy Torres November 3, 2025
Box breathing is a gem – simple, structured, and respects limited lung capacity. Try it and feel the difference.
Andrew McKinnon November 7, 2025
Look, the jargon isn’t just for show; the autonomic shift from sympathetic to parasympathetic is a real, measurable change. When you employ mindful pauses, you’re essentially dialing down the fight‑or‑flight cascade that tightens the airways. So, while the buzzwords sound flashy, they map onto concrete physiological pathways.
Dean Gill November 10, 2025
Embarking on a mindfulness journey as an emphysema patient can feel like stepping into uncharted territory, but the evidence accumulated over the past decade paints a hopeful picture. First, numerous randomized controlled trials have demonstrated that regular meditation reduces cortisol levels, which in turn mitigates inflammatory processes that exacerbate lung tissue damage. Second, the practice of focused breathing teaches the nervous system to recognize false alarms, thereby preventing unnecessary spikes in heart rate and respiratory effort that often accompany panic. Third, patients who engage in daily mindfulness report a subjective improvement in quality of life, citing better sleep, reduced fatigue, and a calmer outlook on their condition. Fourth, the simplicity of short, 5‑minute sessions lowers the barrier to entry, making it feasible even for those with severe breathlessness who cannot commit to lengthy exercises. Fifth, clinicians have begun to incorporate mindfulness questionnaires into routine assessments, allowing objective tracking of anxiety and stress alongside spirometry. Sixth, the synergistic effect of combining pulmonary rehabilitation with mindfulness appears to amplify the benefits of each modality, as the physical conditioning reduces baseline breathlessness while the mental training curtails the emotional response to dyspnea. Seventh, mindfulness encourages patients to adopt a more proactive stance toward their health, shifting the narrative from passive suffering to active management. Eighth, group meditation sessions foster community support, which itself is a protective factor against depression in chronic illness. Ninth, the neuroplastic changes observed in brain imaging studies suggest that sustained practice can rewire the fear circuitry associated with breathlessness, making patients less reactive over time. Tenth, the cost‑effectiveness of mindfulness programs, often delivered via free apps, makes them accessible to a wide demographic without adding financial strain. Eleventh, while improvements in FEV1 are modest, they are statistically significant and consistent across multiple cohorts. Twelfth, the reduction in emergency department visits reported in several observational studies underscores the real‑world impact of these interventions. Thirteenth, the practice does not replace pharmacotherapy; rather, it complements inhaler use by potentially reducing the frequency of rescue medication needed. Fourteenth, families and caregivers also benefit, as they observe calmer interactions and fewer crisis moments. Finally, the cumulative evidence supports the notion that mindfulness and meditation, when tailored to the constraints of emphysema, serve as a valuable adjunct in comprehensive disease management.
Royberto Spencer November 11, 2025
While the enumeration of benefits is impressive, one must caution against over‑promising outcomes to vulnerable patients. The modest gains in lung function should be framed realistically, lest hope turn into disappointment. Moreover, adherence remains a challenge; without sustained effort, the physiological changes revert. Nonetheless, integrating these practices responsibly can enrich the therapeutic landscape.
Annette van Dijk-Leek November 15, 2025
Okay, folks, here’s the thing: you don’t need a PhD in neuroscience to start breathing mindfully, you just need a few minutes and a willingness to try, and honestly, the results can be surprisingly uplifting, especially when you track them, because data doesn’t lie, it tells you what’s working, and when you see that your anxiety scores are dropping, you’ll feel validated, so go ahead, give it a shot, and watch the transformation unfold!
Katherine M November 16, 2025
Absolutely! 🎉 The data you collect becomes a personal progress chart, and sharing a celebratory emoji can reinforce the positive habit loop. Keep it up, and let those little victories pile up! 🌟
Bernard Leach November 20, 2025
The practical aspect of mindfulness for emphysema hinges on three core principles first consistency second breath awareness third integration with existing therapy each principle interacts with the others to create a synergistic effect that can be observed both subjectively and objectively in clinical settings patients who maintain a daily routine of even five minutes report lower anxiety levels and modest improvements in spirometric measurements while clinicians note fewer acute exacerbations and reduced reliance on rescue inhalers the key is to personalize the practice select techniques that respect the patient’s pulmonary limitations for example box breathing or guided body scans that do not demand deep inhalations and to embed the sessions within the patient’s daily schedule such as during morning coffee or before bedtime this approach not only enhances adherence but also fosters a sense of control over a condition that can otherwise feel overwhelming
Shelby Larson November 23, 2025
Listen, the science is clear: mindfulness isn’t a fad it's a validated adjunct therapy. The recent studies, especially the 2024 trial, showed a 12% drop in IL‑6 levels among COPD participants. If you ignore that data, you’re basically turning your back on evidence‑based care. So, stop the nonsense and give it a try.
Mark Eaton November 27, 2025
Great summary, totally agree.