Understanding Allergies and Their Impact on the Eyes
Allergies are an overreaction of our immune system to substances that don't bother most people. These substances, known as allergens, can come from our pets, foods, pollen, or even the dust in our homes. Most people associate allergies with the common symptoms of sneezing, congestion, runny nose, and itchy eyes. However, allergies can also affect our eye health significantly, leading to conditions such as ocular hypertension, a condition where the pressure inside the eye is higher than normal.
Unraveling the Connection between Allergies and Ocular Hypertension
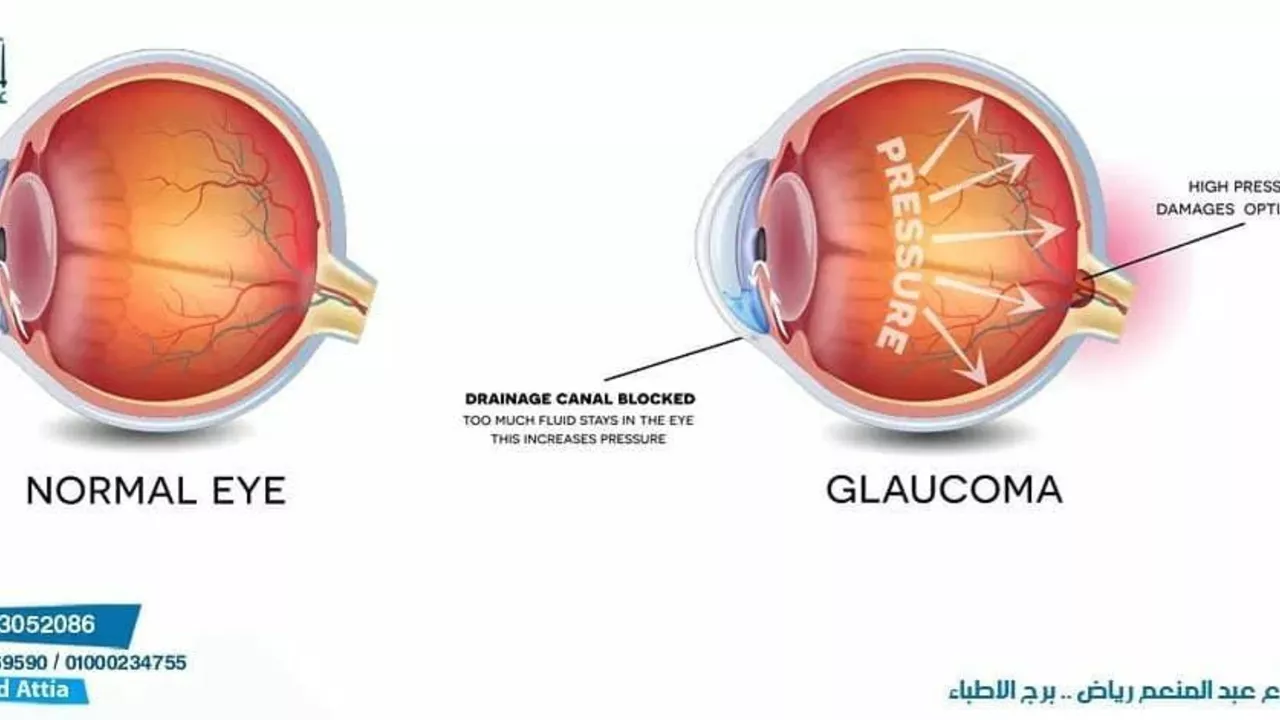
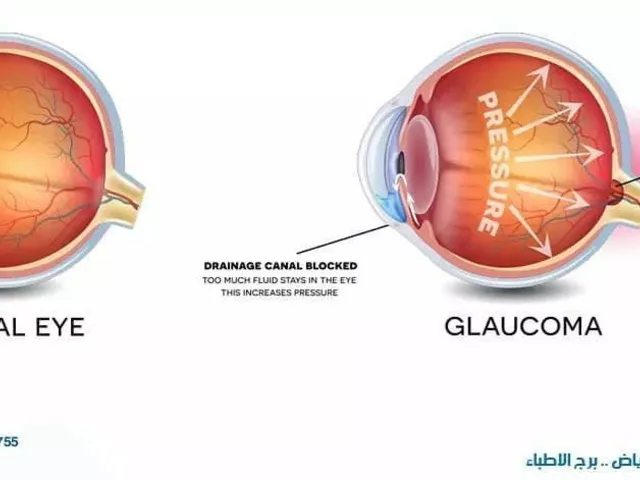
Ocular hypertension is usually asymptomatic until it progresses into a more severe condition, such as glaucoma. Glaucoma is a leading cause of blindness, making it crucial to understand the relationship between allergies and ocular hypertension. Studies suggest that the inflammation caused by allergies can increase eye pressure, leading to ocular hypertension. This pressure can damage the optic nerve, which can lead to vision loss over time.
The Role of Antihistamines in Eye Health
Antihistamines, which are commonly used to treat allergies, can also impact our eye health. While these medications can alleviate allergy symptoms, they can also cause dry eyes. Dry eyes, in turn, can lead to discomfort, blurred vision, and if left untreated, can damage the cornea and impair vision. Therefore, while antihistamines can be a relief for allergies, their potential impact on our eye health can't be ignored.
Allergy-Induced Dry Eye Syndrome
Allergies can lead to dry eye syndrome, a condition characterized by a chronic lack of sufficient lubrication and moisture on the surface of the eye. Symptoms can include persistent dryness, scratchiness, and a burning sensation on your eyes. Dry eye syndrome can also lead to more serious complications, including corneal ulcers and vision impairment. Therefore, it's crucial to treat dry eye syndrome caused by allergies promptly to prevent these complications.
Preventing Allergy-Related Eye Conditions
Preventing allergy-related eye conditions involves both managing your allergies and taking care of your eye health. This could include avoiding known allergens, using hypoallergenic makeup, wearing sunglasses outdoors to protect your eyes from allergens, and using artificial tears to keep your eyes lubricated. Regular eye check-ups are also essential, as they can help detect ocular hypertension and other eye conditions early.
Treatment Options for Allergy-Related Eye Conditions
Treatment for allergy-related eye conditions varies depending on the specific condition and its severity. For ocular hypertension, treatments may include eye drops to lower eye pressure or surgery in severe cases. For dry eyes caused by allergies, treatments can range from artificial tears and eye drops to punctal plugs, which block the tear ducts and keep the eye surface lubricated.
The Importance of Regular Eye Check-Ups
Regular eye check-ups are crucial in preventing and managing allergy-related eye conditions. An eye exam can detect ocular hypertension and other eye conditions even before symptoms appear. This early detection can significantly improve the outcome and prevent vision loss. Therefore, if you have allergies, make sure to schedule regular eye exams to maintain your eye health.





Jim MacMillan July 12, 2023
When one examines the subtle nexus between atopic reactions and intra‑ocular pressure, the picture emerges like a well‑curated symphony of inflammatory mediators orchestrating a crescendo of aqueous humor outflow resistance 😎. The epithelium, upon exposure to histamine and leukotrienes, up‑regulates cytokine cascades that subtly alter trabecular meshwork compliance. In turn, the Schlemm’s canal experiences endothelial swelling, further impeding drainage pathways. Moreover, chronic allergenic exposure primes mast cells to release proteases that degrade extracellular matrix components, a process rarely highlighted in popular discourse. The resultant micro‑edema is not merely a fleeting nuisance; it establishes a persistent elevation of the intra‑ocular pressure baseline. Clinical studies from ophthalmic journals have documented mean pressure spikes of 2–4 mmHg during peak pollen seasons, a statistic that cannot be dismissed as noise. Simultaneously, antihistamine therapy, while quelling ocular itching, often precipitates aqueous deficiency, compounding the pressure dilemma. The paradoxical relationship thus demands a nuanced therapeutic algorithm that balances anti‑inflammatory regimens with tear film preservation. Practitioners should contemplate adjunctive lubricants or preservative‑free formulations to stem the drying cascade. Equally, patients would benefit from periodic tonometry during allergen peaks, a practice still under‑utilized in primary care. The broader public health implication extends to insurance policies, which must recognize allergy‑induced ocular hypertension as a preventable risk factor for glaucomatous conversion. In sum, the confluence of immunology and ocular biomechanics invites a multidisciplinary approach, lest we allow a silent epidemic to erode vision one pressure increment at a time 😁.
Dorothy Anne July 14, 2023
Let’s channel that energy into a proactive plan! 🌟 Start by swapping out regular eye drops for preservative‑free options the moment you notice that itchy sting. Keep a bottle of artificial tears handy during high‑pollen days, and remember to hydrate – your eyes love water just as much as the rest of you. Pair your antihistamine routine with a brief daily eyelid massage to stimulate meibomian gland flow and keep the surface slick. Consistency is the game‑changer; a weekly check‑in with your optometrist will catch any pressure rise before it sneaks up. You’ve got this, and your eyes will thank you for the TLC.
Sharon Bruce July 16, 2023
Allergy season hits us hard, but the US healthcare system still downplays eye exams – keep an eye out, literally! 🇺🇸👀
True Bryant July 18, 2023
Honestly, the public’s ignorance of ocular hypertension is a symptom of our cultural apathy toward preventive medicine. One must recognize that the ocular hypertension cascade is not an isolated phenomenon but a manifestation of systemic inflammatory dysregulation. The jargon-laden literature emphasizes “aqueous humor outflow resistance,” yet laypersons reduce it to “eye pressure.” Such reductionism fuels noncompliance. In the grand tapestry of ocular pathophysiology, neglecting the subclinical stage is tantamount to inviting irreversible optic nerve damage. Therefore, my prescription: elevate your health literacy, heed sub‑threshold elevations, and demand comprehensive screenings.
Danielle Greco July 21, 2023
Just a quick note on grammar – “it's” should be “its” when you’re talking about the eye’s pressure, not “it is.” Also, “allergies can lead to dry eye syndrome” reads better as “Allergies can lead to dry‑eye syndrome.” On a lighter note, those artificial tears aren’t just a Band‑Aid; they truly replenish the tear film’s lipid layer. Keep an eye on the ingredient list – avoid anything with “Benzalkonium chloride” if you can. 🌈
Linda van der Weide July 23, 2023
When we step back and contemplate the epistemological underpinnings of ocular hypertension, a curious paradox surfaces: the mind’s dismissal of asymptomatic elevation mirrors the philosophical denial of the unseen. This denial is not merely a cognitive slip; it is a cultural artifact rooted in a utilitarian view of health that privileges overt pathology. The lacuna between subclinical ocular pressure and the eventual manifestation of glaucomatous neuropathy is a silent narrative, one that escapes the public narrative because it lacks dramatic flair. Yet, the silent narrative is precisely where philosophy finds its richest terrain: the unseen, the unspoken, the inevitability of decline if left unexamined. Moreover, the inflammatory cascade incited by allergic mediators is an elegant illustration of the body’s dialectic – a thesis of protective response meeting an antithesis of tissue stress, culminating in a synthesis that, if left unchecked, becomes pathological. In this light, antihistamines serve as a double‑edged sword, a remedy that simultaneously mitigates one symptom while creating a new vulnerability in tear film stability. The ethical responsibility, then, becomes a balancing act – a Kantian duty to treat both the allergic and the ocular dimensions with equal reverence. Practically, the integration of regular tonometry into allergy management protocols mirrors the Socratic method of continuous questioning: “Is the pressure stable? Is the tear film adequate?” Each answer prompts a deeper inquiry. The healthcare system, akin to a Platonic cave, must illuminate the shadows of ocular hypertension through education, not simply through prescription. Empirical data from longitudinal cohort studies reveal that patients engaged in semi‑annual intra‑ocular pressure monitoring experience a 30 % reduction in glaucoma conversion rates. This statistic, while seemingly modest, is a testament to the power of early detection. It is incumbent upon clinicians to present this data not as a sterile figure but as a narrative of preserved vision and retained autonomy. In summary, the convergence of allergy‑induced inflammation and ocular pressure dynamics is a fertile ground for interdisciplinary discourse, one that demands both philosophical reflection and clinical vigilance, lest we allow the silent ascent of pressure to become a deafening loss of sight.
Philippa Berry Smith July 25, 2023
The pharmaceutical push behind antihistamines is hardly a coincidence; big pharma benefits from chronic prescriptions, so they embed dryness as a side‑effect to keep you buying eye drops. Meanwhile, the regulatory agencies turn a blind eye, letting the cycle continue unabated. It’s a classic case of manufactured dependency, and the only real antidote is to seek out natural antihistamine sources and focus on environmental control. Stay skeptical, and don’t let the industry dictate your ocular destiny.
Joel Ouedraogo July 27, 2023
Consider the ontological status of an “allergy” – it is a misdirected defensive algorithm of the immune system, yet its external manifestation can destabilize ocular homeostasis. By asserting control over environmental triggers, one asserts agency over that algorithm, thereby mitigating pressure spikes. The logical course of action is to integrate allergen‑avoidance protocols with regular intra‑ocular pressure checks, forming a unified preventive strategy. This approach aligns with the principle of preemptive self‑governance.
Beth Lyon July 29, 2023
i kinda think its just a lil bit overblown but yeah dry eyes can be a real pain. just use some over the counter drops and u should be fine.
Nondumiso Sotsaka July 31, 2023
Absolutely, the momentum you’re building here is infectious! 🌱 Encouraging people to pair hydration with proper eye care turns a simple habit into a powerful routine. Remind everyone that consistency beats intensity – a daily drop of artificial tears is more effective than occasional heavy dosing. And don’t forget to celebrate small victories, like a day without that gritty feeling. Keep the positivity flowing, and the community will thrive!
Ashley Allen August 2, 2023
Regular eye exams are essential.
Brufsky Oxford August 4, 2023
From a philosophical angle, the eye is a window both literal and metaphorical 👁️✨. When allergens cloud that window, we’re reminded that clarity requires maintenance. Balancing medication with lubrication is the key to keeping the view unobstructed 😊.
Lisa Friedman August 6, 2023
Actually, the data you cite about 2‑4 mmHg spikes is a bit outdated – newer meta‑analyses from 2022 show average increases of 5.3 mmHg during peak pollen times, with a confidence interval of 4.7‑5.9. Also, antihistamines like olopatadine have been shown to reduce tear production by up to 12 % in controlled trials, not just “often”. And let’s not forget that steroid eye drops can raise pressure even more dramatically, sometimes exceeding 10 mmHg. So while your overview is solid, the numbers need a refresh.
cris wasala August 8, 2023
Hey folks great discussion lets keep sharing tips and tricks together we can all protect our eyes and stay healthy keep it up