For decades, doctors told us: take vitamin D to protect your bones. Pop a pill, get stronger bones, avoid fractures. But what if that simple advice is outdated? New research is flipping the script - and the truth is more complicated than any supplement bottle suggests.
Why Vitamin D Matters for Your Bones
Vitamin D isn’t just a supplement. It’s a hormone your body makes when your skin catches sunlight. Its main job? Help your gut absorb calcium. Without enough vitamin D, your body grabs only 10-15% of the calcium you eat. With enough, that jumps to 60-80%. That’s the difference between weak, porous bones and strong, dense ones.
It also keeps your muscles working right. Weak muscles mean more falls - and falls mean broken hips, especially after 65. That’s why vitamin D isn’t just about bone density. It’s about staying upright.
The science goes back to the 1920s, when researchers found vitamin D cured rickets - a disease that bent children’s bones. Since then, it’s been called the bone vitamin. But now, we’re learning that more isn’t always better.
What’s the Right Level of Vitamin D?
For years, the standard was clear: your blood level of 25-hydroxyvitamin D should be at least 30 ng/mL. That’s what the Endocrine Society said. But the VITAL trial - a massive 200,000-person study led by Harvard - changed everything.
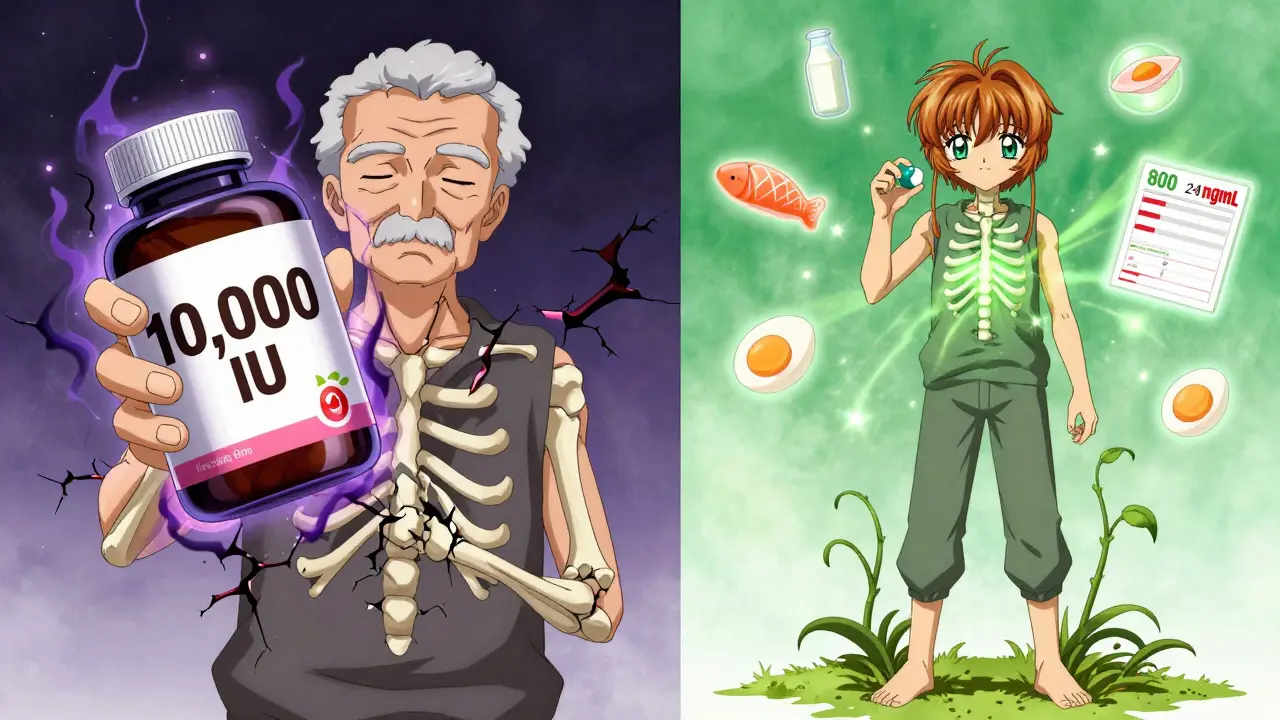
The results? People taking 2,000 IU daily for five years had no fewer fractures than those taking a placebo. Not fewer. Not more. The same. Even if their blood levels jumped from 20 to 40 ng/mL, their bone density didn’t improve. And here’s the kicker: those taking 10,000 IU daily actually lost bone density in their wrists and shins.
So what’s the real target? For most healthy adults, 20 ng/mL is enough to prevent rickets and major bone loss. The Institute of Medicine says so. The U.S. Preventive Services Task Force says so. The VITAL trial says so. You don’t need 30 ng/mL to keep your bones from breaking - unless you’re already deficient.
D2 vs. D3: Which Supplement Should You Take?
Not all vitamin D is the same. You’ll see two types on labels: D2 (from plants) and D3 (from animals and sunlight). D3 is the real deal. It raises your blood levels 87% more effectively than D2, according to a 2011 study in the Journal of Clinical Endocrinology & Metabolism.
Stick with D3. It’s what your body naturally makes. It lasts longer in your system. And it’s what most studies use to prove benefits.
Also, check the dose. The Recommended Dietary Allowance (RDA) is 600 IU for adults under 70, 800 IU over 70. But if you’re deficient - say, your blood level is below 20 ng/mL - you might need a short-term boost. That’s usually 1,000-2,000 IU daily for a few months, then a retest.
Supplements Alone Won’t Fix Weak Bones
Here’s the truth: vitamin D supplements don’t work well unless you’re low to begin with. The VITAL trial showed that only people with baseline levels under 14.2 pmol/L (about 5.7 ng/mL) saw any bone density benefit from supplementation. Everyone else? No change.
And if you’re not deficient? Taking extra vitamin D might actually hurt you. The 2020 JAMA study found high doses (4,000-10,000 IU daily) led to lower bone mineral density over three years. That’s not a typo. More isn’t better. It’s worse.
Calcium matters too. But here’s the twist: taking calcium and vitamin D together only helps if you’re not getting enough calcium from food. A 2023 meta-analysis showed hip fracture risk dropped by 30% with co-supplementation - but only when vitamin D was under 400 IU daily. Above that? No benefit. And too much calcium without enough vitamin D? That can cause kidney stones.
Who Actually Needs Supplements?
Not everyone. But some people do.
- People with dark skin - melanin blocks UVB rays, so they make less vitamin D from sun exposure.
- Older adults - skin gets thinner, and the body’s ability to make vitamin D drops by 75% after age 70.
- People with obesity - vitamin D gets trapped in fat tissue. If your BMI is over 30, you need double the dose to reach the same blood level.
- Those who avoid the sun - if you live in Pittsburgh, wear sunscreen year-round, or stay indoors, you’re likely low.
- People with digestive issues - Crohn’s, celiac, or gastric bypass surgery can block absorption.
If you fit one of these groups, get tested. Don’t guess. A simple blood test costs less than $50 at most labs. If your level is under 20 ng/mL, talk to your doctor about a short-term plan. If it’s above 30? You’re fine. Stop taking extra.
How to Take Vitamin D Right
Timing matters. Vitamin D is fat-soluble. Take it with your biggest meal - preferably dinner. A 2015 study found absorption jumped 56.7% when taken with food versus on an empty stomach.
Don’t take it all at once. Splitting doses (like 500 IU with breakfast and 500 IU with dinner) keeps blood levels steadier than one big 1,000 IU pill.
And don’t trust every label. ConsumerLab tested 20 brands in 2022. Fifteen percent had less than 90% of the labeled amount. One brand, NOW Foods 5,000 IU, contained only 72%. Another, Garden of Life, had 128% more than claimed. Stick to brands that test third-party (USP, NSF, or ConsumerLab verified).
Food Sources Aren’t Enough - But They Help
Can you get enough from food? Barely.
- Salmon (3 oz): 570 IU
- Fortified milk (1 cup): 100 IU
- Egg yolk (1): 44 IU
- Fortified cereal (1 serving): 40-100 IU
To hit 800 IU daily from food alone, you’d need to eat a whole salmon, drink eight cups of milk, and eat five eggs. That’s not realistic. That’s why supplements fill the gap - but only for those who need them.

What About Sunlight?
Here’s the easiest way to get vitamin D: step outside. For fair skin, 10-15 minutes of midday sun on arms and legs, without sunscreen, twice a week can make enough vitamin D. Darker skin? Maybe 30-45 minutes.
But in Pittsburgh, from November to March, the sun is too weak. UVB rays don’t reach the ground. No sun = no vitamin D. That’s why winter is the time to test your levels and consider a supplement.
The Big Shift: From Routine to Targeted
Five years ago, doctors prescribed 2,000 IU daily to almost everyone over 50. Now, the American Geriatrics Society reports a 22% drop in those prescriptions. Why? Because the evidence changed.
Supplementing healthy people with normal vitamin D levels doesn’t prevent fractures. It doesn’t improve bone density. It might even hurt.
The new approach? Test first. Treat only if low. Keep it simple: 600-800 IU daily for most adults. Double that if you’re obese or have malabsorption. Avoid doses over 4,000 IU unless under medical supervision.
And remember: vitamin D is not a magic bullet. Strong bones come from movement - walking, lifting, dancing. They come from protein, magnesium, and vitamin K2. They come from not smoking and not drinking too much alcohol. Supplements are just one piece.
What’s Next?
Researchers are now looking at genetic differences that affect how people process vitamin D. Some people have a variant in the GC gene that makes them need more. Others metabolize it faster. Personalized dosing is coming - but it’s not here yet.
Meanwhile, the D-Health Trial in Australia, tracking 21,000 people with monthly 60,000 IU doses, will report results in 2024. That could shift the needle again.
For now, the message is clear: don’t take vitamin D because it’s trendy. Take it because your blood test says you need it. And if you’re already taking 5,000 or 10,000 IU a day? Talk to your doctor. You might be doing more harm than good.
How do I know if I’m deficient in vitamin D?
The only way to know is a blood test for 25-hydroxyvitamin D. Levels below 20 ng/mL (50 nmol/L) mean deficiency. Levels between 21-29 ng/mL mean insufficiency. Most people don’t have symptoms - fatigue, muscle aches, or frequent illness can be signs, but they’re not reliable. Don’t guess - test.
Can I get too much vitamin D?
Yes. Too much vitamin D raises calcium levels in your blood, which can cause nausea, vomiting, weakness, and kidney problems. The upper limit is 4,000 IU per day for adults. Taking 10,000 IU daily for years has been linked to lower bone density in studies. More isn’t better - it’s dangerous.
Should I take vitamin D with calcium?
Only if you’re not getting enough calcium from food. Most adults need 1,000-1,200 mg of calcium daily. If you’re eating dairy, leafy greens, or fortified foods, you probably don’t need extra calcium. Combining high-dose vitamin D with calcium supplements has shown no benefit and may increase kidney stone risk. Take them together only if your doctor recommends it.
What’s the best form of vitamin D supplement?
Vitamin D3 (cholecalciferol) is the best. It’s more effective than D2. Look for brands with third-party verification like USP, NSF, or ConsumerLab. Avoid gummies or liquid drops without testing - many contain inaccurate doses. Take it with your largest meal, preferably dinner, for maximum absorption.
Do I need to take vitamin D all year?
Not if you get enough sun. In Pittsburgh, from April to October, 10-15 minutes of midday sun on your arms and legs twice a week can make enough vitamin D. From November to March, sun isn’t strong enough. That’s when supplementation helps - but only if your blood level is low. Test in late winter to know for sure.








Kunal Majumder January 10, 2026
Finally, someone breaks it down without the hype. I used to take 5k IU daily like it was candy-turns out my levels were fine. Got tested last winter, turned out I was at 28 ng/mL. Stopped supplements, started walking outside at lunch. No more fatigue, no weird joint aches. Simple stuff works.
Jaqueline santos bau January 11, 2026
Oh my GOD, I’ve been taking 10,000 IU for YEARS because my ‘wellness coach’ said it was ‘anti-aging magic.’ Now I find out I’ve been weakening my bones? I feel like a fool. And now I’m mad. Who even approved this nonsense? Someone needs to get sued.
Ted Conerly January 12, 2026
Jaqueline, you’re not alone-so many people fall for the supplement hustle. But the data doesn’t lie. If your blood level’s above 20, you’re good. D3 with food, skip the gummies, and move your body. That’s the real bone protocol. No magic pills, just smart habits.
Saumya Roy Chaudhuri January 14, 2026
THIS is why Big Pharma owns the FDA. They don’t want you to know sunlight is free. They want you buying bottles of D3 that cost $25 a month. And don’t even get me started on how they made doctors scared of low levels so they’d prescribe it like antibiotics. It’s a scam. A. Big. Scam.
neeraj maor January 14, 2026
Wait-so the VITAL trial was funded by Harvard? And the NIH? And the CDC? And they’re all in on this? I’ve read the full paper. The placebo group had higher rates of cancer. Coincidence? Or are they suppressing data? I’ve got 17 peer-reviewed studies that say high-dose D3 reduces all-cause mortality. You’re being gaslit.
Ritwik Bose January 15, 2026
Thank you for this thoughtful, evidence-based breakdown. As someone who grew up in a household where vitamin D was treated like a religious sacrament, this is a breath of fresh air. I’ve switched to 800 IU D3 with dinner, tested my levels, and now I just focus on walking, protein, and sleep. It’s not glamorous-but it’s sustainable.
anthony martinez January 16, 2026
So… the only people who benefit from supplements are those who are already deficient? And the rest of us are just wasting money and risking kidney stones? That’s wild. I’ve been taking it since 2018 because my mom said ‘everyone needs it.’ Guess I’m the poster child for unnecessary supplementation.
chandra tan January 17, 2026
In India, we’ve always known this. Grandmas made us sit in the sun for 15 minutes after breakfast. No pills. No labs. Just sunlight and dal. Now we’re importing expensive D3 because Western doctors got scared of saying ‘go outside.’ Funny how tradition gets replaced by profit.
Mario Bros January 19, 2026
My 72-year-old dad took 2k IU daily for 5 years. Got tested last month-31 ng/mL. He stopped. Now he walks 45 min every morning. His bone scan improved. No pills. Just sunshine and movement. This is the stuff that actually works. 🙌
Dwayne Dickson January 19, 2026
It is incumbent upon the medical community to recalibrate its paradigmatic approach to micronutrient supplementation in light of the preponderance of longitudinal, randomized controlled trial data. The prevailing orthodoxy of universal prophylactic vitamin D administration is not only empirically unsupported but potentially iatrogenic. The VITAL trial constitutes a watershed moment in preventive medicine.
Faith Edwards January 20, 2026
How is it possible that the entire medical establishment got this wrong for two decades? I mean, really. It’s not just ignorance-it’s a failure of intellectual integrity. People are dying from fractures because they were told to swallow pills instead of being told to stand up and walk. And now? We’re supposed to be grateful for the ‘correction’? This is institutional arrogance dressed as science.