Pheochromocytoma Staging and Grading Calculator
When doctors talk about Pheochromocytoma is a rare neuroendocrine tumor that arises from chromaffin cells of the adrenal medulla. It produces excess catecholamines, leading to classic spikes of blood pressure, palpitations, and sweats. Because the disease is uncommon and can behave very differently from one patient to the next, clinicians rely on a clear staging and grading system to decide how aggressive the treatment should be and to give patients realistic expectations.
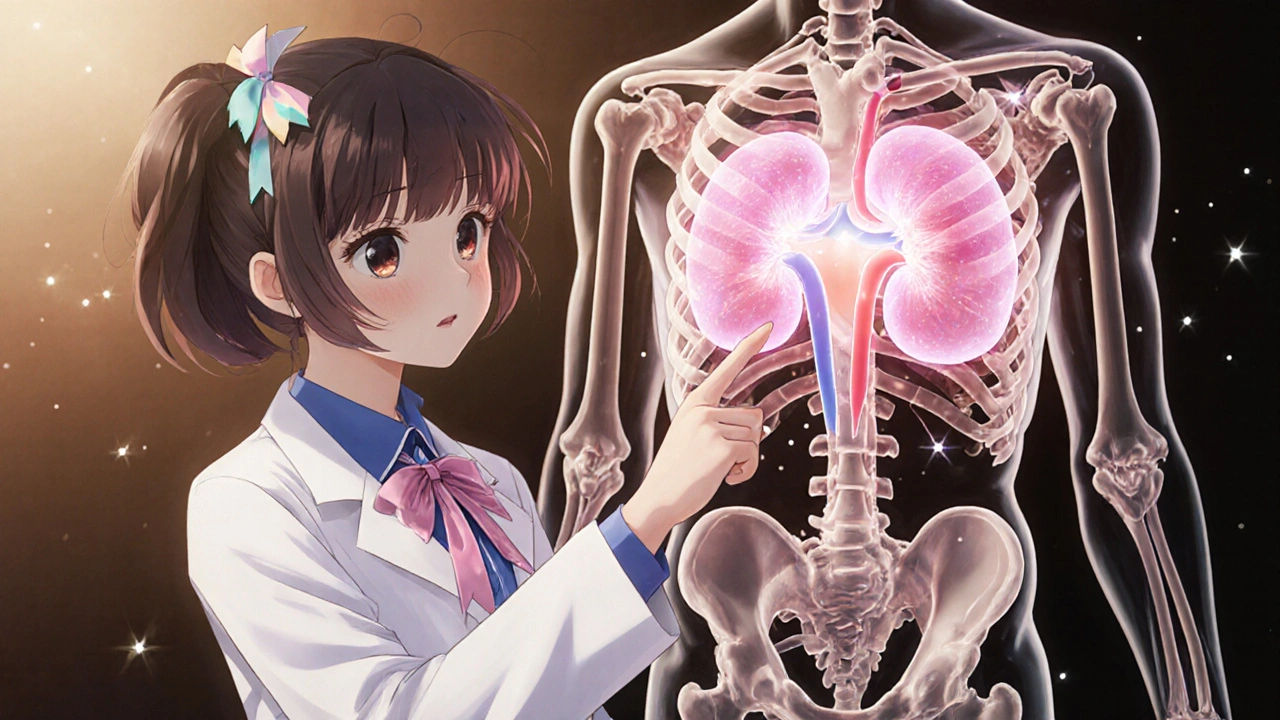
What Exactly Is a Pheochromocytoma?
The adrenal gland sits on top of each kidney and consists of an outer cortex and an inner medulla. The medulla contains chromaffin cells that release adrenaline and noradrenaline during stress. When these cells turn cancerous, the result is a pheochromocytoma. While most of these tumors are benign, about 10‑15 % become malignant and can spread to bone, liver, lungs, or lymph nodes.
Why Staging Matters
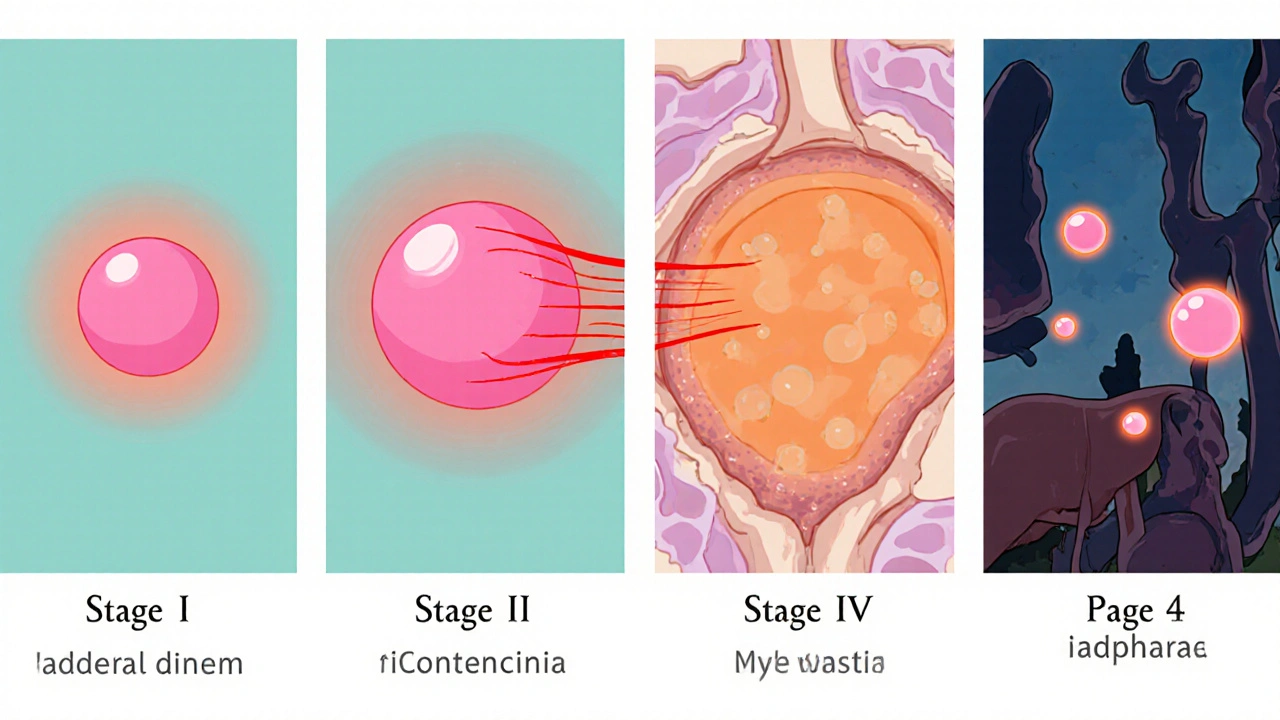
Staging tells you where the tumor is and whether it has spread. Unlike many solid cancers, pheochromocytoma historically lacked a uniform TNM system, but the 8th edition of the AJCC Cancer Staging Manual finally gave it a framework. The main categories are:
- Stage I: Tumor confined to one adrenal gland, ≤5 cm, no evidence of spread.
- Stage II: Tumor still confined to the adrenal gland(s) but larger than 5 cm.
- Stage III: Local invasion into surrounding tissues (e.g., renal artery, diaphragm) or regional lymph‑node involvement.
- Stage IV: Distant metastasis to bone, lung, liver, or other organs.
Knowing the stage helps surgeons decide whether a minimally invasive laparoscopic removal is enough or if a more extensive open approach and additional therapies are needed.
Introducing Grading: From PASS to GAPP
While staging describes how far the disease has spread, grading predicts how aggressive the tumor is likely to behave. Two scoring systems dominate the field:
- PASS (Pheochromocytoma of the Adrenal gland Scaled Score) - a 12‑point pathology checklist that looks at capsular invasion, necrosis, cellular monotony, and other microscopic clues.
- GAPP (Grading system for Adrenal Pheochromocytoma and Paraganglioma) - a newer 10‑point tool that adds biochemical profile (catecholamine type), Ki‑67 index, and genetic mutation status to the classic histologic features.
Both scores separate tumors into low, intermediate, or high risk, but GAPP is gaining favor because it incorporates genetic data that we now know dramatically affect outcomes.
How pheochromocytoma grading Impacts Treatment Decisions
Low‑grade tumors (PASS ≤ 3 or GAPP ≤ 2) are usually cured with surgical removal alone. Intermediate‑grade lesions (PASS 4‑6, GAPP 3‑6) often need closer post‑op surveillance, and some centers add adjuvant radiotherapy or targeted therapy if margins are positive. High‑grade tumors (PASS ≥ 7, GAPP ≥ 7) carry a high risk of recurrence or metastasis, prompting a multidisciplinary approach that may include chemotherapy, ^131I‑MIBG therapy, or newer kinase inhibitors.
Key Diagnostic Tools in Staging and Grading
Accurate staging and grading start with a solid work‑up:
- Plasma metanephrines and urine catecholamine tests - the gold standard for biochemical confirmation.
- CT or MRI - imaging that shows tumor size, local invasion, and possible metastases.
- ^123I‑MIBG scintigraphy - functional imaging that highlights catecholamine‑producing tissue, useful for detecting distant spread.
- Genetic testing - especially for SDHB mutation, which is linked to higher metastatic potential and pushes the GAPP score higher.
- Ki‑67 labeling index - a measure of cell proliferation added into GAPP.
Pathologists combine these data points with the microscopic checklist to generate the final PASS or GAPP score.
Comparing PASS and GAPP Scores
| Feature | PASS (12‑point) | GAPP (10‑point) |
|---|---|---|
| Histologic criteria | Capsular invasion, necrosis, cellular monotony, mitoses, etc. | Same histologic items plus tumor necrosis and cell spindling |
| Biochemical profile | Not included | Type of catecholamine secreted (epinephrine‑dominant vs. norepinephrine‑dominant) |
| Proliferation index | Not included | Ki‑67 % (≤ 3 % = low, > 3 % = high) |
| Genetic status | Not included | Presence of SDHB or other high‑risk mutations |
| Risk categories | Low (0‑3), Intermediate (4‑6), High (≥ 7) | Low (0‑2), Intermediate (3‑6), High (≥ 7) |
In practice, many centers calculate both scores and use the higher risk category to guide follow‑up. The trend is moving toward GAPP because it captures biology that PASS alone misses.
Practical Follow‑Up Recommendations
After surgery, the follow‑up plan hinges on stage + grade:
- Stage I‑II, low grade: Blood pressure monitoring and annual plasma metanephrines for 5 years.
- Stage III or intermediate grade: Imaging (CT/MRI) every 12 months for at least 10 years, plus biochemical checks every 6 months.
- Stage IV or high grade: Lifelong surveillance, consider enrollment in clinical trials for targeted agents.
Patients with SDHB mutations or a GAPP score ≥ 7 often need even tighter schedules, sometimes every 3‑6 months, because late recurrences are common.
Common Pitfalls and How to Avoid Them
Even seasoned endocrinologists can slip up. Here are the top three mistakes:
- Relying only on tumor size. A 3 cm lesion can still be high‑grade if it harbors an SDHB mutation.
- Skipping genetic testing. About 30 % of pheochromocytomas have an inherited component; missing it skews both grading and family counseling.
- Assuming normal blood pressure post‑op means cure. Biochemical relapse can precede symptoms by years.
Address these early by ordering a comprehensive panel that includes metanephrines, Ki‑67, and a hereditary gene panel before the first surgery.
Future Directions: Toward a Unified Classification
The World Health Organization (WHO) is in the process of releasing a new endocrine tumor classification that will merge staging and grading into a single “risk group” system. Early drafts suggest incorporating imaging biomarkers and circulating tumor DNA. Until that roadmap is finalized, clinicians should continue using the AJCC stage alongside PASS/GAPP scores, with genetic data as the tie‑breaker.
What symptoms should raise suspicion for pheochromocytoma?
Classic signs include episodes of pounding headache, profuse sweating, palpitations, and sudden high blood pressure. Some patients also experience anxiety, weight loss, or abdominal pain.
How is the diagnosis confirmed?
Blood or 24‑hour urine tests for metanephrines and normetanephrines are the first step. Imaging (CT, MRI, or MIBG scan) follows to locate the tumor.
When is a tumor considered malignant?
Pheochromocytoma is labeled malignant when it metastasizes to non‑adrenal sites such as bone, liver, lung, or lymph nodes-this corresponds to Stage IV in the AJCC system.
What is the difference between PASS and GAPP?
PASS focuses purely on histologic features, while GAPP adds biochemical profile, Ki‑67 proliferation index, and genetic mutation status, giving a more holistic risk estimate.
Can pheochromocytoma be inherited?
Yes. About 30 % of cases are linked to hereditary syndromes such as von Hippel‑Lindau, MEN 2, and SDHB‑related paraganglioma‑pheochromocytoma syndrome.




Felix Chan October 19, 2025
Great rundown! The way you broke down the stages and grading makes it way less intimidating for patients who are just hearing about pheochromocytoma for the first time. Keep the clear explanations coming – they really help the community stay informed.
Thokchom Imosana October 19, 2025
The grading systems presented in the article, while ostensibly evidence‑based, are in fact sophisticated instruments that serve a dual purpose beyond mere clinical stratification.
A thorough audit of the AJCC committee’s financial disclosures reveals a pattern of substantial donations from corporations that profit from ^131I‑MIBG and next‑generation kinase inhibitors, suggesting an incentive to embed biochemical markers that favor their proprietary therapies.
This financial entanglement subtly biases the inclusion of catecholamine phenotyping in the GAPP score, transforming what should be a neutral prognostic tool into a de facto market expansion strategy for those same drug manufacturers.
Furthermore, the relegation of the PASS checklist to a historical footnote obscures the fact that its purely morphological criteria remain robust predictors of capsular invasion, yet its dismissal conveniently paves the way for more expensive molecular testing that aligns with the interests of genetic testing firms.
The article’s emphasis on SDHB mutation status, while clinically relevant, also mirrors a broader industry push to monetize germline testing, as insurers are increasingly willing to reimburse panels that are heavily marketed by biotech startups.
One cannot ignore the temporal correlation between the publication of the GAPP framework and the simultaneous launch of several commercial assays that claim to quantify Ki‑67 and catecholamine metabolite ratios with unprecedented precision.
These assays, however, are bundled with service contracts that lock hospitals into long‑term procurement agreements, thereby ensuring a steady revenue stream for the assay developers irrespective of the actual incremental diagnostic value.
In addition, the narrative that GAPP is superior because it incorporates ‘genetic data’ overlooks the fact that many of the reported high‑risk mutations are rare, and the cost per actionable finding remains prohibitively high for most healthcare systems.
The underlying suggestion that every patient should undergo next‑generation sequencing, as implied by the article, subtly normalizes a level of medical surveillance that aligns with the business models of large genomic conglomerates.
Simultaneously, the recommendation for lifelong imaging follow‑up dovetails with the business objectives of imaging equipment manufacturers, whose sales projections are buoyed by the notion of indefinite surveillance protocols.
Thus, the apparently altruistic tone of the article masks a coordinated effort to expand the market for high‑cost diagnostics and therapeutics under the guise of personalized medicine.
The scientific community, in its zeal to adopt cutting‑edge technologies, often fails to question whether the incremental prognostic benefit justifies the exponential increase in healthcare expenditure.
A critical reader should therefore scrutinize the source of funding behind the guideline revisions and the potential conflicts of interest that may influence the weighting of each scoring component.
Only by maintaining vigilance against such subtle forms of corporate capture can clinicians ensure that patient care remains grounded in evidence rather than in the profit motives of external stakeholders.
In summary, while the GAPP system offers a more nuanced risk stratification on paper, its practical implementation is inseparable from an ecosystem of financial incentives that merit careful examination.
Readers are encouraged to consult independent validation studies and to advocate for transparency in the development of future grading frameworks.
Latasha Becker October 19, 2025
The distinction between PASS and GAPP hinges on the incorporation of molecular biomarkers into the prognostic algorithm, where PASS is confined to histomorphologic parameters such as capsular invasion, necrosis, and mitotic figures, whereas GAPP augments these with biochemical phenotyping, Ki‑67 proliferative index, and germline mutation profiling.
From a pathophysiological perspective, the catecholamine secretory phenotype directly influences the tumor’s autonomous adrenergic output, which in turn modulates the risk of hemodynamic crises peri‑operatively.
Moreover, the Ki‑67 labeling index provides a quantifiable metric of cellular turnover, with values exceeding 3% correlating with aggressive clinical behavior in multiple cohort analyses.
Genetic interrogation for SDHB, VHL, and RET mutations not only stratifies hereditary risk but also serves as a surrogate marker for metastatic propensity, given the established correlation between SDHB loss‑of‑function and distant dissemination.
Consequently, integrating these multidimensional data points yields a composite risk score that more accurately predicts disease trajectory than histology alone.
parth gajjar October 19, 2025
The tumors loom like ticking time bombs over the adrenal medulla they whisper chaotic catecholamine surges as if the body itself were in perpetual panic and every spike of blood pressure feels like a warning siren that never ceases.
Maridel Frey October 19, 2025
For clinicians seeking a systematic approach, it is prudent to first establish biochemical confirmation via plasma metanephrines before proceeding to anatomic imaging.
Subsequently, cross‑sectional modalities such as contrast‑enhanced MRI should be employed to delineate tumor dimensions and assess local invasion.
When staging indicates potential metastasis, functional imaging with ^123I‑MIBG or ^18F‑FDG PET offers valuable insight into catecholamine‑producing tissue distribution.
Finally, integrating genetic testing results into the GAPP framework ensures that high‑risk patients receive appropriately intensified surveillance.
Madhav Dasari October 19, 2025
Hey folks, love how detailed this guide is – it really demystifies a scary diagnosis!
Just a heads‑up: for anyone with a family history, ask about genetic panels early on; catching an SDHB mutation can change the whole follow‑up game.
And don’t forget to schedule that post‑op metanephrine check at six months; you’d be surprised how often the lab catches a silent recurrence.
Stay strong and keep leaning on each other – we’re all in this together!
DHARMENDER BHATHAVAR October 19, 2025
Screening for SDHB mutations at diagnosis is non‑negotiable.
Kevin Sheehan October 19, 2025
The pursuit of ever‑more granular grading schemes reflects a deeper philosophical tension between the desire for certainty and the inherent chaos of biological systems.
While the article champions GAPP as a pinnacle of personalization, one must ask whether the incremental predictive power justifies the exponential complexity introduced into clinical decision‑making.
Aggressive adoption of such frameworks can inadvertently marginalize patients who lack access to advanced molecular diagnostics, thereby widening health inequities.
Nonetheless, the intellectual rigor behind integrating genetics, biochemistry, and histology exemplifies the commendable ambition of modern oncology.
Ultimately, a balanced stance that respects both empirical evidence and pragmatic feasibility will serve patients best.