Introduction to Tranexamic Acid
As someone who has closely followed developments in the medical field, I've seen the dramatic impact of tranexamic acid on preventing postpartum hemorrhage. Tranexamic acid, or TXA, is a medication often used in surgery to prevent excessive blood loss. Over time, it has shown great potential in the field of obstetrics, specifically in preventing postpartum hemorrhage - a leading cause of maternal mortality worldwide.
It's essential to understand that TXA works by stopping the breakdown of blood clots, which can be lifesaving during clinical procedures. As a blogger, I feel it's crucial to delve deeper into this topic and explore the significant role that TXA plays in saving lives.
How Tranexamic Acid Prevents Postpartum Hemorrhage
One of the key aspects of TXA is its effectiveness in preventing postpartum hemorrhage. Postpartum hemorrhage, also known as PPH, is excessive bleeding after childbirth. PPH can be life-threatening and is a significant cause of maternal mortality globally.
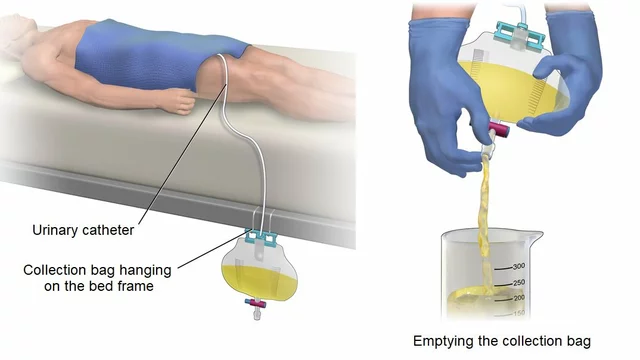
Tranexamic acid has shown promise in preventing this. The medication works by inhibiting the enzymes that dissolve blood clots, thus reducing the chances of heavy bleeding. It's interesting to note that TXA can be administered both orally and intravenously, giving healthcare providers flexible options depending on the patient's condition.
Research and Studies on Tranexamic Acid
Now, let's talk about the research and studies on TXA. Several studies have been conducted to evaluate the effectiveness of TXA in preventing postpartum hemorrhage. One of the most notable is the WOMAN trial, which involved over 20,000 women from 21 countries.
The results of the WOMAN trial were significant. The study found that early administration of TXA reduced the risk of death due to bleeding by nearly one-third. This is a remarkable finding and has led to the increased use of TXA in managing postpartum hemorrhage.
Benefits and Risks of Tranexamic Acid
While TXA has proven beneficial, it's equally important to discuss the potential risks. Like any medication, TXA has its side effects. Some patients may experience nausea, vomiting, and diarrhea. In rare cases, the drug can cause blood clots, leading to serious complications like strokes or pulmonary embolisms.
However, these risks are relatively low compared to the potential benefits of TXA. By reducing the risk of postpartum hemorrhage, TXA can significantly lower maternal mortality rates, particularly in low-resource settings where access to emergency obstetric care may be limited.
Future of Tranexamic Acid in Obstetric Care
Finally, let's look to the future. The role of TXA in preventing postpartum hemorrhage is a promising one. As more research is conducted, we can expect to see increased use of this medication in obstetric care.
It's exciting to think about the potential impact of TXA on maternal health. By reducing the risk of postpartum hemorrhage, we can move closer towards the global goal of reducing maternal mortality. As a blogger, I look forward to keeping you updated on this critical advancement in women's healthcare.






Tyler Johnson July 6, 2023
Reading through the latest data on tranexamic acid (TXA) really underscores how far obstetric care has come in the fight against postpartum hemorrhage. The WOMAN trial, which enrolled over twenty thousand women across twenty‑one countries, demonstrated a roughly one‑third reduction in death due to bleeding when TXA was administered early. This is not a marginal benefit; it translates into thousands of lives saved each year, especially in low‑resource settings where access to rapid surgical intervention is limited. From a pharmacological standpoint, TXA’s inhibition of plasminogen activation preserves clot integrity, allowing the uterine vessels to seal more effectively after delivery. Moreover, the drug’s safety profile is reassuring: while nausea and occasional vomiting are reported, the incidence of serious thrombotic events remains low, particularly when used within the recommended dosing window. It is also worth noting that TXA can be given both intravenously and orally, offering flexibility in different clinical environments. The oral formulation could be a game‑changer for community health workers who need a portable solution for women delivering at home. In terms of implementation, WHO’s recommendation to use TXA within three hours of birth aligns well with existing emergency obstetric protocols, making integration relatively seamless. Training programs that emphasize early recognition of postpartum hemorrhage and prompt TXA administration could further amplify the drug’s impact. Additionally, cost‑effectiveness analyses suggest that TXA is inexpensive compared to the economic burden of managing severe hemorrhage and its complications. Future research should continue to explore optimal dosing strategies, especially in populations with co‑morbidities such as anemia or pre‑eclampsia, to fine‑tune safety. There is also a growing interest in assessing TXA’s role in preventing hemorrhage in other obstetric scenarios, like placenta previa or uterine atony, which could broaden its utility. Overall, the evidence is compelling: tranexamic acid stands as a critical tool in our armamentarium against maternal mortality, and its wider adoption could bring us significantly closer to global health targets.
Annie Thompson July 6, 2023
Honestly the way TXA works is kind of magical – it just stops the clots from breaking down and you can literally see the difference in blood loss when it’s given early. The data from the WOMAN trial really blew my mind because a one‑third reduction in death is huge and it’s something we can actually apply in the field. It’s also comforting that the side effects are generally mild and not something that would outweigh the benefits in a desperate situation.
Parth Gohil July 7, 2023
From a clinical pharmacology perspective, the mechanism of TXA – inhibition of the lysine‑binding sites on plasminogen – is a solid example of targeted therapy that aligns well with obstetric emergency protocols. In practice, administering a 1 g IV dose within the three‑hour window can be seamlessly integrated into existing massive transfusion algorithms, especially in tertiary centers. Moreover, the pharmacokinetic profile, featuring a half‑life of roughly two hours, supports repeat dosing in cases of ongoing hemorrhage without significant accumulation. This synergy between pharmacodynamics and clinical workflow makes TXA a low‑hanging fruit for resource‑constrained settings looking to improve maternal outcomes.
VAISHAKH Chandran July 7, 2023
TXA is over‑hyped many people ignore the rare clotting risks it can cause especially in patients with underlying coagulopathies its use should be more selective.
Pat Merrill July 7, 2023
Oh great another "miracle drug" – yeah TXA does help but let’s not pretend it’s a silver bullet for everything. The side‑effects aren’t just nausea, there are cases of serious thrombo‑embolic events that get swept under the rug. And sure, the cost is low, but you can’t just dump it everywhere without proper training – otherwise you’ll have a new set of problems. *sigh*
Vicki Roth July 7, 2023
Interesting point, but I think the overall benefit outweighs the risks.
Vishal Bhosale July 7, 2023
TXA works, it’s cheap, and doctors like it. No need to overthink it.
Garima Gauttam July 7, 2023
Actually i think relying on TXA alone is naive it can’t replace good obstetric care and proper monitoring.
Georgia Nightingale July 7, 2023
Wow, drama alert! TXA is the superhero we needed but also the villain when misused. It’s like a double‑edged sword – on one side it slashes mortality, on the other it can cause a cascade of complications if you don’t follow protocols. Honestly, the hype is justified, but the cautionary tales are real. So, bravo to the researchers, but let’s keep the hype in check!
Chris Kivel July 7, 2023
I’ve seen TXA used in a few clinics here and it really does cut down on blood loss. The key is getting it in fast, within that three‑hour window, and making sure the staff are trained.
sonia sodano July 7, 2023
Honestly I think the whole TXA craze is just another medical fad – we’ll see a decade later if it truly makes a difference or if it’s just a convenient talking point for pharma.