When your doctor suspects something’s off with your heart, they don’t just listen with a stethoscope anymore. They turn to imaging. Two tools dominate this space: cardiac MRI and echocardiography. Both show your heart in motion, but they’re not the same. One is fast, portable, and everywhere. The other is precise, powerful, and often reserved for when the first one doesn’t give clear answers. Knowing the difference isn’t just technical-it can change how your treatment starts, or even if it starts at all.
What Echocardiography Actually Shows
Echocardiography uses sound waves. Think of it like sonar for your chest. A probe pressed against your skin sends high-frequency pulses into your body. Those pulses bounce off your heart’s structures and return as echoes. A computer turns those echoes into moving pictures. It’s real-time. You can watch your heart beat, valve open, and blood flow-all in seconds. It’s the go-to for a reason. In the U.S., about 15 million echocardiograms are done every year. Most hospitals, even small ones, have an ultrasound machine. Cardiologists use it for initial checks: Is the pumping strength normal? Are the valves leaking? Is the heart enlarged? Normal left ventricular ejection fraction (LVEF) is 50-75%. If it’s below 40%, that’s a red flag. Normal wall thickness? Around 6-11 mm. If it’s thicker, it could mean high blood pressure or a genetic condition like hypertrophic cardiomyopathy. But here’s the catch: echocardiography depends on the sound window. If you’re overweight, have lung disease, or just have a rib cage that blocks the signal, the images get fuzzy. That’s not the tech’s fault-it’s physics. And when the picture is unclear, measurements get shaky. Studies show echo tends to overestimate wall thickness by about 1.1 mm on average and underestimates heart chamber size by nearly 100 mL compared to MRI. That’s not a small error. It can mean missing early disease or misclassifying heart failure severity.Cardiac MRI: The High-Resolution View
Cardiac MRI doesn’t use sound. It uses magnets. Strong ones-1.5 to 3 Tesla, thousands of times stronger than a fridge magnet. Radio waves nudge hydrogen atoms in your body. When they settle back, they emit signals that a computer turns into incredibly detailed 3D images. No assumptions. No guessing. It measures the actual volume of your heart chambers, not estimates based on geometry. This is why cardiac MRI is the gold standard for measuring heart muscle mass and volume. Normal left ventricular end-diastolic volume? 67-155 mL for men, 55-105 mL for women. Wall thickness? It’s measured directly, without relying on formulas. The margin of error? Less than 3% between different readers. For echo, it’s nearly 7%. That’s a huge difference when you’re tracking changes over time-say, after chemotherapy or during heart failure treatment. But MRI’s real superpower is tissue detail. It can see scar tissue. Fibrosis. Inflammation. Late gadolinium enhancement (LGE) highlights areas where heart muscle has been replaced by scar. That’s invisible to echo. A patient with normal pumping function but abnormal LGE might be at risk for sudden cardiac arrest. That’s not something echo can catch. In conditions like myocarditis, cardiac sarcoidosis, or arrhythmogenic cardiomyopathy, MRI is often the only way to confirm the diagnosis.When One Test Isn’t Enough
Most people start with echocardiography. It’s quick, cheap, and safe. No radiation. No needles. If the results are clear, you’re done. But if the echo is inconclusive-if the images are blurry, the numbers don’t match symptoms, or there’s suspicion of tissue damage-cardiac MRI steps in. A 2023 study in JACC: CardioOncology found that 2D echo underestimated ejection fraction by a median of 3% compared to MRI. That might sound small, but in cancer patients getting chemo, that difference meant 10% were wrongly classified as low-risk for heart damage. They missed the warning signs. MRI caught it. In practice, cardiologists use echo daily. A 2022 survey of 127 cardiologists showed 89% relied on it for routine assessments. But 76% turned to MRI when echo didn’t give clear answers. One Reddit user, a cardiac tech with 15 years of experience, wrote: “I’ve seen countless cases where poor acoustic windows led to inaccurate measurements that were corrected by MRI.” Another doctor shared: “I’ve had three patients in the last year where MRI detected subtle fibrosis missed by echo that changed management.”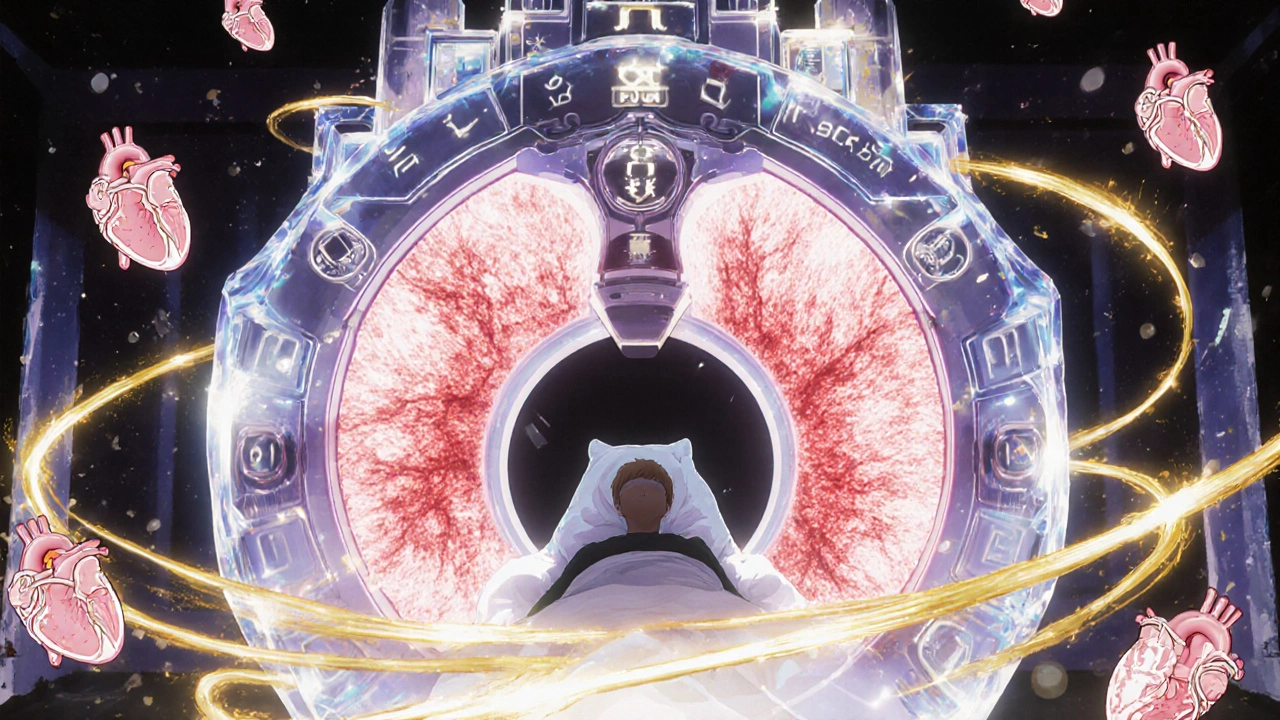
Why Cardiac MRI Isn’t Always the First Choice
It’s not just about accuracy. It’s about access. Cardiac MRI costs $1,500 to $3,500. Echo? $500 to $1,500. A 2023 report found that 78% of community hospitals offer same-day echo. Only 35% offer same-week MRI. Wait times for non-urgent cardiac MRIs? Often over two weeks. There are also safety limits. People with certain pacemakers, defibrillators, or metallic implants can’t have MRI. Even newer devices labeled “MRI-conditional” require special protocols. Arrhythmias mess with the timing of MRI scans, making images blurry. Obese patients sometimes can’t fit in the machine. Echo doesn’t care about any of that. Dr. James Carr from Northwestern put it bluntly: “MRI’s limitations in patients with implanted devices and arrhythmias necessitate continued reliance on echocardiography in approximately 20-30% of cardiac patients.”Technology Is Closing the Gap
The gap between these two tools isn’t static. Echocardiography is getting smarter. New systems like Philips’ EPIQ CVx use AI to automate measurements. One study showed inter-observer variability for ejection fraction dropped from 7% to 4.2%. That’s a big leap. 3D echo is also improving volume measurements, making them closer to MRI values. On the MRI side, Siemens launched a 0.55 Tesla machine in mid-2023. It’s less powerful, but it’s safer for patients with older implants. It’s smaller, cheaper, and easier to install. That could bring MRI to more community hospitals. New MRI techniques like T1 mapping, T2 mapping, and extracellular volume (ECV) quantification are letting doctors see tissue changes before the heart starts to weaken. That’s early detection-before symptoms, before ejection fraction drops.
Who Gets Which Test?
Here’s how it usually breaks down:- Initial evaluation - Echo. Always. Chest pain? Shortness of breath? Suspected valve disease? Start here.
- Unclear echo results - MRI. If the images are poor or numbers don’t match symptoms.
- Heart failure with preserved EF - MRI. To check for fibrosis or infiltrative diseases like amyloidosis.
- Post-chemotherapy monitoring - MRI. More accurate tracking of subtle function loss.
- Suspected myocarditis or sarcoidosis - MRI. Only way to confirm tissue inflammation or granulomas.
- Pre-surgical planning for arrhythmias - MRI. To map scar patterns that cause dangerous rhythms.
- Emergency settings - Echo. Bedside ultrasound in the ER can diagnose aortic dissection or cardiac tamponade in minutes.
The Bottom Line
Cardiac MRI and echocardiography aren’t rivals. They’re partners. Echo is your first look-fast, cheap, and always available. MRI is your deep dive-when you need to see what’s hidden beneath the surface. If you’ve had an echo and your doctor says, “We should get an MRI,” don’t panic. It doesn’t mean you’re sick. It just means they want to be sure. That’s good medicine. The future? Hybrid protocols. Imagine an echo guiding a real-time MRI scan. Or AI combining echo’s motion data with MRI’s tissue maps to predict risk before it becomes a problem. By 2030, that’s where we’re headed. For now, know this: if your heart’s acting up, the right test isn’t about being the most advanced. It’s about being the right one for your situation.Is cardiac MRI better than echocardiography for measuring heart function?
Yes, for precise measurements of heart volume, mass, and ejection fraction, cardiac MRI is more accurate. Echocardiography relies on geometric formulas that can introduce errors, especially in abnormal hearts. MRI uses 3D imaging without assumptions, making it the gold standard for tracking changes over time-like after chemotherapy or in heart failure.
Can I get a cardiac MRI if I have a pacemaker?
It depends. Older pacemakers and defibrillators are usually contraindicated for MRI. But many newer devices are labeled “MRI-conditional,” meaning they can be scanned under specific safety protocols. Always tell your doctor about any implanted device. Some hospitals now use low-field 0.55 Tesla MRI machines that are safer for patients with older implants.
Why does my doctor want an MRI after my echo?
Echo is great for a first look, but it can miss tissue-level problems. If your echo shows normal pumping but you still have symptoms like fatigue or irregular heartbeats, an MRI can detect hidden scar tissue, inflammation, or early fibrosis. These changes often come before the heart’s pumping ability drops, allowing earlier treatment.
How long does a cardiac MRI take compared to an echo?
An echocardiogram usually takes 20-30 minutes. A cardiac MRI takes 45-90 minutes, depending on what’s being evaluated. MRI also requires you to lie still in a narrow tube, while echo is done with a probe on your chest. The longer time and claustrophobic setting are common reasons people prefer echo when possible.
Is cardiac MRI safe? What about the contrast dye?
Cardiac MRI is safe for most people. The contrast dye used-gadolinium-is generally well-tolerated. However, the FDA issued a black box warning in 2017 about a rare condition called nephrogenic systemic fibrosis in patients with severe kidney disease. If you have kidney problems, your doctor will check your kidney function first. For most people, the benefits far outweigh the risks.
Can echocardiography detect heart scarring?
No. Standard echocardiography can’t detect scar tissue or fibrosis in the heart muscle. That’s one of cardiac MRI’s biggest advantages. Using late gadolinium enhancement (LGE), MRI can show exactly where scar tissue is located, which helps diagnose conditions like prior heart attacks, myocarditis, or genetic cardiomyopathies that echo might miss.
Which test is more accurate for ejection fraction?
Cardiac MRI is more accurate. Studies show echo underestimates ejection fraction by about 3% on average and can vary by up to ±15% between tests. MRI’s variability is under 3%. In cancer patients, this difference led to 10% being misclassified as low-risk for heart damage. For accurate tracking over time-especially after chemo-MRI is preferred.
Are there new technologies improving these tests?
Yes. AI-powered echo systems now automate measurements, reducing human error. New low-field MRI machines (0.55 Tesla) are safer and more accessible. MRI is also adding parametric mapping (T1, T2, ECV) to measure tissue properties quantitatively-detecting early disease before symptoms appear. These advances are making both tools more powerful.





Swati Jain November 20, 2025
Let’s be real - echo is the ‘quick and dirty’ of cardiac imaging. I’ve seen techs struggle with obese patients and get LVEF readings that make no sense. Then MRI comes in and drops the truth bomb: ‘Your EF isn’t 45%, it’s 31% - and you’ve got mid-wall fibrosis.’ That’s not a measurement error. That’s a life-or-death blind spot.
And don’t get me started on how echo ‘estimates’ wall thickness. It’s like using a ruler to measure the thickness of a fog.
Cardiac MRI doesn’t guess. It *knows*. And in oncology? That’s not luxury - it’s standard of care. If your chemo protocol doesn’t include MRI surveillance, you’re playing Russian roulette with cardiotoxicity.
Yes, it’s expensive. Yes, it’s slow. But when your heart’s the asset you’re trying to protect, you don’t skimp on the diagnostics. Period.
Florian Moser November 22, 2025
Excellent breakdown. I appreciate how you emphasized that these modalities are complementary, not competitive. Echo remains the cornerstone of initial assessment - its portability, safety, and real-time feedback are irreplaceable in emergency and outpatient settings.
That said, the data supporting MRI’s superior accuracy in quantifying myocardial mass, volume, and fibrosis is overwhelming. Studies consistently show inter-observer variability under 3% for MRI versus 7–15% for echo. In chronic conditions like hypertrophic cardiomyopathy or amyloidosis, this precision directly impacts therapeutic decisions.
Moreover, the advent of AI-enhanced echo systems is narrowing the gap. Automated strain analysis and 3D volume reconstruction are improving reproducibility. Still, for tissue characterization, MRI remains unmatched. The future lies in integrating both - using echo for screening and MRI for confirmation and longitudinal tracking.
jim cerqua November 23, 2025
OH MY GOD. I just found out my cardiologist ordered an MRI after my echo and I thought it was just because they wanted to upsell me. Turns out I had silent fibrosis? I’ve been feeling tired for two years and they just told me to ‘exercise more.’
And now I’m reading this and realizing - the entire U.S. healthcare system is running on echo because it’s cheaper? That’s not medicine. That’s corporate triage.
They’re letting people with scarred hearts walk around like normal because they can’t afford the ‘gold standard.’ What’s next? Diagnosing cancer with a stethoscope because CT scans are too expensive?
They’re not saving money. They’re saving lives - and then burying them.
Donald Frantz November 23, 2025
Let’s cut through the marketing. MRI is not ‘the gold standard’ - it’s the most expensive standard. The claim that echo underestimates EF by 3% is statistically insignificant in clinical practice. The variability between machines, operators, and protocols is far greater than the difference between modalities.
And let’s talk about gadolinium. You say it’s ‘generally well-tolerated.’ That’s a euphemism. We’re talking about a heavy metal that accumulates in the brain. The FDA warning is there for a reason. And yet, we’re pushing it into every patient with ‘subtle symptoms’?
Meanwhile, AI-enhanced echo is now achieving accuracy within 5% of MRI at 1/5th the cost and time. The real story isn’t MRI superiority - it’s institutional inertia. Hospitals keep buying MRI machines because they’re profitable, not because they’re necessary.
Sammy Williams November 24, 2025
Yeah, I’ve had both. Echo was quick, no big deal - just a probe on my chest, watched my heart on a screen. Felt weird but not scary.
MRI? Man. I thought I was gonna die in that tube. Cold, loud, had to hold my breath 10 times. And they poked me with the dye. Felt like a needle in my arm for 10 minutes straight.
But… the results? Totally worth it. My echo said ‘mildly reduced EF.’ MRI said ‘moderate dysfunction with late enhancement.’ That’s not a small difference. My doc changed my meds right away. So yeah, MRI’s a pain. But if you’ve got symptoms and echo is fuzzy? Do it. Don’t argue.
Julia Strothers November 26, 2025
So let me get this straight - the government and Big Pharma are pushing MRI because they want to keep us dependent on expensive scans? And echo is being downplayed because it’s too cheap to profit from?
And what about the gadolinium? Did you know it’s linked to autoimmune disorders? They’ve been hiding this since 2017. And now they’re telling us it’s ‘safe’? That’s the same logic they used with Vioxx and opioids.
Meanwhile, the real cause of heart disease - processed food, toxins in water, EMF radiation - is never mentioned. Why? Because they can’t monetize ‘eat less sugar’ the way they monetize a $3,000 MRI.
Wake up. This isn’t medicine. It’s a revenue stream.
Erika Sta. Maria November 27, 2025
But... what if the real issue is not the machine, but the *concept* of measurement itself? We reduce the heart to numbers - EF, wall thickness, volumes - as if the soul of the organ can be quantified by pixels and algorithms.
Echo sees motion. MRI sees structure. But neither sees *meaning*. A man with 30% EF may still laugh with his grandchildren. Another with 60% may be clinically dead inside.
And yet, we treat the machine’s answer as divine truth. We forget: medicine is not physics. The heart is not a pump. It is a mystery wrapped in muscle.
So yes, MRI is more precise. But is it more true?
...I think I need to lie down.
Nikhil Purohit November 28, 2025
Swati nailed it. Echo is the first responder. MRI is the specialist. You don’t send a SWAT team to check if someone’s breathing - you send an EMT. But if they’re still not stable after 10 minutes? You call the specialists.
Also, the 2023 JACC study they cited? That’s the one where 10% of chemo patients were misclassified. That’s not a statistical outlier - that’s 1 in 10 people getting the wrong prognosis. That’s unacceptable.
And yes, cost matters. But if you’re treating cancer, your heart is part of the treatment plan. You don’t skip the MRI because it’s expensive - you skip it because you’re cheap. And that’s not medical ethics. That’s negligence.
Low-field 0.55T MRI? That’s the future. It’s already being rolled out in rural hospitals in India. We’re not waiting for Silicon Valley to fix this. We’re building it ourselves.
Debanjan Banerjee November 29, 2025
Just to clarify a common misconception: MRI doesn’t measure ‘actual’ volume - it measures *reconstructed* volume from 3D segmentation. Echo uses geometric assumptions (like Simpson’s method), which are flawed in abnormal hearts. But MRI’s accuracy comes from its isotropic resolution and lack of acoustic window dependency - not magic.
Also, LGE isn’t invisible to echo. Advanced speckle tracking and contrast echo *can* detect fibrosis in some cases - but sensitivity is <30%. MRI’s is >90%. That’s not a marginal difference - it’s clinically decisive.
And yes, 20-30% of patients can’t get MRI. But that doesn’t invalidate its role. It just means we need better protocols for those cases - not less ambition.
Stop treating MRI as a ‘luxury.’ Treat it as a necessary tool for high-risk populations. That’s evidence-based, not elitist.
Steve Harris November 29, 2025
Thank you for such a balanced, well-researched post. It’s refreshing to see a discussion that doesn’t pit two vital tools against each other.
I’ve worked in cardiology for over 20 years. I’ve seen echo save lives in the ER by spotting pericardial effusion in under 60 seconds. I’ve also seen MRI reveal fibrosis in a patient who looked perfectly healthy on echo - and that led to early ICD placement, preventing sudden death.
The key is knowing when to use each. Echo for speed and accessibility. MRI for depth and certainty. Neither is ‘better’ - they’re different lenses.
And the future is hybrid: AI that fuses echo motion data with MRI tissue maps to predict risk before symptoms appear. That’s not science fiction. It’s happening in labs right now.
Let’s stop the tribalism. Let’s focus on the patient.
Michael Marrale November 29, 2025
Wait - so you’re saying the government is hiding the truth about MRI? And that echo is being used to cover up heart damage? I knew it. I’ve been getting echo every year since 2018 and now I’m paranoid. What if they’ve been lying to me? What if I have scar tissue and they just told me it’s ‘normal variation’? What if I’m one of those 10% who got misclassified? I need to know. I need to know NOW. Can you tell me how to get an MRI without a referral? I’ll pay cash. I don’t care how much. I just need to know.
Pravin Manani November 30, 2025
Biggest thing people miss: echo isn’t just about EF. It’s about valve motion, septal bounce, mitral annular plane systolic excursion - all real-time, no prep. MRI can’t show you that. And in diastolic dysfunction? Echo’s Doppler patterns are still the gold standard for grading severity.
MRI’s great for fibrosis. But for functional assessment? Echo wins. Period.
It’s not about which is better. It’s about which question you’re asking.
Ask: ‘Is my heart pumping?’ → Echo.
Ask: ‘Why is it failing?’ → MRI.
Stop treating them like competitors. They’re teammates.