Quick Takeaways
- Empagliflozin lowers blood sugar and cuts heart‑failure risk better than many older drugs.
- Canagliflozin and dapagliflozin share the same class benefits but differ in kidney safety and dosing.
- Metformin remains the cheapest first‑line option but lacks the strong heart‑protective data.
- GLP‑1 agonists like liraglutide offer weight loss and cardiovascular gain at a higher price.
- Choosing the right drug depends on kidney function, heart disease history, cost, and personal preferences.
When it comes to type‑2 diabetes, the market is crowded with pills, injections, and pumps. Empagliflozin has risen to prominence because it not only drops glucose levels but also shows a solid track record for heart‑failure protection. This article walks you through a side‑by‑side look at Empagliflozin and its most common alternatives, so you can see which fits your health goals, budget, and lifestyle.
What is Empagliflozin?
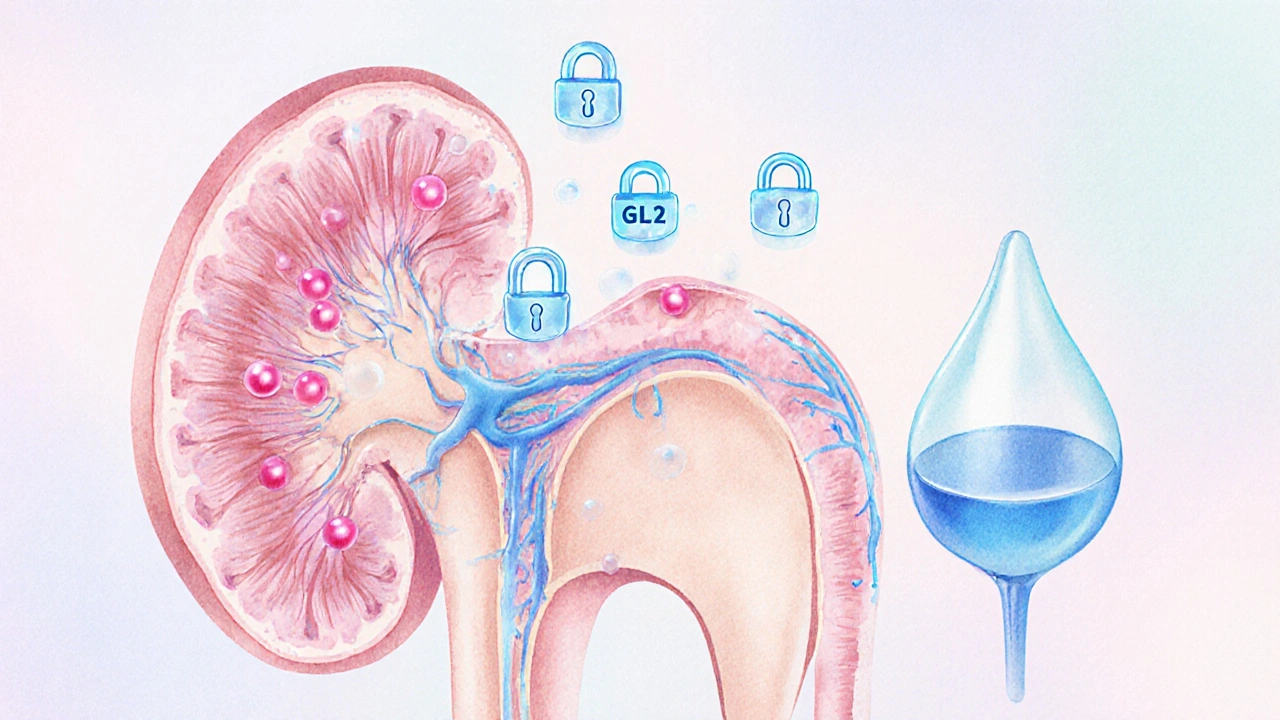
Empagliflozin belongs to the class of drugs called SGLT2 inhibitors. It works by blocking the sodium‑glucose co‑transporter‑2 proteins in the kidney, forcing excess glucose out through urine. Approved by the FDA in 2014, the medication is sold under the brand name Jardiance and is taken once daily.
How Empagliflozin Works - The Science in Plain English
The kidneys filter about 180liters of blood each day. In people with diabetes, they re‑absorb too much glucose. Empagliflozin shuts the re‑absorption gate, so glucose leaves the body. The result is lower HbA1c (a measure of average blood sugar), modest weight loss, and less fluid overload - a key factor in heart‑failure.
Key Benefits of Empagliflozin
- HbA1c reduction: typically 0.7‑0.9%.
- Cardiovascular outcomes: EMPA‑REG OUTCOME trial showed a 38% cut in cardiovascular death.
- Kidney protection: slows eGFR decline in patients with chronic kidney disease.
- Weight loss: average 2‑3kg over a year.
- Convenient dosing: once‑daily oral tablet.
How We Compare Diabetes Drugs
To make the comparison useful, we look at five practical dimensions:
- Mechanism of action - how the drug lowers glucose.
- Efficacy - average HbA1c drop.
- Cardiovascular & kidney impact - major outcomes from large trials.
- Side‑effect profile - common and serious safety concerns.
- Cost & insurance coverage - average wholesale price (AWP) in the United States.
Side‑by‑Side Comparison Table
| Drug | Class | FDA Approval (yr) | Avg HbA1c ↓ | Cardio/Kidney Benefit | Common Side‑effects | US Avg Monthly Cost* |
|---|---|---|---|---|---|---|
| Empagliflozin | SGLT2 inhibitor | 2014 | 0.7‑0.9% | ↓38% CV death; slows eGFR loss | UTI, genital infection, dehydration | $350 |
| Canagliflozin | SGLT2 inhibitor | 2013 | 0.6‑0.8% | ↓27% CV death; reduces albuminuria | UTI, amputation risk (rare), bone fracture | $370 |
| Dapagliflozin | SGLT2 inhibitor | 2014 | 0.5‑0.7% | ↓17% CV death; renal protection in CKD | UTI, genital infection, volume depletion | $340 |
| Metformin | Biguanide | 1995 (US) | 0.8‑1.0% | No proven CV benefit; modest renal safety | GI upset, B12 deficiency | $4 |
| Liraglutide | GLP‑1 receptor agonist | 2010 (US) | 1.0‑1.5% | ↓22% CV death; weight loss 5‑6kg | Nausea, pancreatitis (rare) | $900 |
*Prices reflect average wholesale cost; actual out‑of‑pocket can vary.
Deep Dive into Each Alternative
Canagliflozin
Canagliflozin is another SGLT2 inhibitor that got a nod a year before Empagliflozin. Its big claim is a reduction in major adverse cardiovascular events (MACE) demonstrated in the CANVAS program. However, clinicians watch its rare association with lower‑leg amputations, especially in patients with peripheral artery disease.
Dapagliflozin
Dapagliflozin shares the same glucose‑excreting action but shines in patients with chronic kidney disease (CKD). The DAPA‑CKD trial showed a 39% drop in the combined outcome of kidney failure, renal death, or sustained eGFR decline. Its side‑effect list is similar to Empagliflozin, making it a solid backup if you have an issue tolerating the latter.
Metformin
Metformin, the workhorse biguanide, still belongs to first‑line guidelines because it’s cheap, safe, and effective. It reduces hepatic glucose production rather than forcing sugar out via urine. While it lacks the robust heart‑failure data of SGLT2 inhibitors, its long‑track record makes it a common companion drug.
Liraglutide (GLP‑1 agonist)
Liraglutide belongs to the GLP‑1 receptor agonist family. Administered by daily injection, it mimics the gut hormone GLP‑1 to boost insulin secretion and curb appetite. The LEADER trial proved a 13% reduction in CV death. The trade‑off: higher price and injection‑related inconvenience.
Choosing the Right Medication for You
There’s no one‑size‑fits‑all answer. Below is a quick decision guide:
- Heart‑failure or ASCVD risk: Empagliflozin or canagliflozin are top picks.
- Chronic kidney disease (eGFR<45): Dapagliflozin has the strongest renal data.
- Budget‑conscious: Metformin wins hands‑down.
- Need weight loss: GLP‑1 agonists like liraglutide out‑perform SGLT2 inhibitors.
- Concern about genital infections: All SGLT2 inhibitors share that risk; discuss hygiene measures with your provider.
Always bring your full medical history to the conversation - especially any history of amputation, severe liver disease, or recurrent urinary infections.
Potential Pitfalls & How to Avoid Them
- Dehydration: SGLT2 inhibitors increase urine output. Stay hydrated, especially in hot weather.
- Ketoacidosis risk: Rare but can happen even with normal glucose. Be alert for nausea, abdominal pain, shortness of breath.
- Drug interactions: Avoid combining SGLT2 inhibitors with high‑dose diuretics without monitoring.
- Cost shock: Check formulary tiers; some insurers list empagliflozin as a specialty tier.
Frequently Asked Questions
Can I take Empagliflozin with Metformin?
Yes. Combining an SGLT2 inhibitor like Empagliflozin with metformin is a common strategy. Metformin tackles liver glucose production while Empagliflozin forces excess glucose out the kidneys, giving a complementary effect on HbA1c.
Do SGLT2 inhibitors cause low blood pressure?
They can lower systolic pressure by a few mmHg because of fluid loss. Most patients tolerate it well, but if you’re already on antihypertensives, your doctor may adjust the dose.
What if I develop a urinary tract infection?
UTIs are the most reported side‑effect. Early treatment with antibiotics usually clears it. Preventive steps include staying hydrated, urinating after sex, and avoiding irritating soaps.
Is Empagliflozin safe for people with moderate kidney disease?
Yes, down to an eGFR of 30mL/min/1.73m². Below that, the glucose‑excreting effect wanes and the label recommends discontinuation.
How does the cost of Empagliflozin compare to GLP‑1 agonists?
Empagliflozin averages $350 per month, while injectable GLP‑1 drugs like liraglutide can exceed $900. Insurance coverage varies, so check your formulary.
Armed with this side‑by‑side view, you can have a more informed chat with your endocrinologist or primary‑care doctor. Remember, the best choice balances effectiveness, safety, and what fits your wallet and lifestyle.
Empagliflozin stands out for heart‑failure protection, but alternatives like canagliflozin, dapagliflozin, metformin, and liraglutide each bring their own strengths. Your personal health profile will dictate which one lands on the front‑runner list.









Jason Oeltjen October 13, 2025
Look, you cant just pick a pill because the ads look snazzy. Empagliflozin might be a wonder drug, but it’s not a free pass to ignore diet and exercise. If you think a pharma company cares about your wallet more than your hearth health, youre right. We need to be morally suparior and demand cheaper options before we throw cash at brand names. Stop letting big pharma decide your life.
Mark Vondrasek October 14, 2025
It’s amazing how the medical community loves to parade the latest SGLT2 inhibitor like it’s a miracle from the lab, while quietly ignoring the cascade of hidden agendas that accompany every new prescription. The FDA approval in 2014 is often cited as a badge of honor, yet no one mentions the behind‑the‑scenes lobbying that paved the way for that badge. Empagliflozin’s cardiovascular numbers look impressive on paper, but remember that the EMPA‑REG trial was funded by the very company that sells Jardiance, so the data can be selectively highlighted. They told us about a 38% reduction in CV death, but conveniently left out the fact that the absolute risk reduction was modest, making the headline look like a Hollywood trailer for a blockbuster that never delivers. Moreover, the side‑effect profile-UTIs, genital infections, dehydration-gets glossed over in the glossy marketing brochures, as if patients can simply ignore a recurring candidiasis infection. And let’s not forget the ever‑present threat of “off‑label” use, where doctors are encouraged to prescribe the drug for conditions it was never rigorously tested for, all under the guise of “clinical innovation.” The hype machinery is powered by relentless direct‑to‑consumer ads that bombard us with images of happy seniors jogging, implying that a single pill can resurrect lost vitality. In reality, these advertisements are designed to manipulate our fear of aging and disease, driving us to buy into a pharmaceutical solution instead of adopting lifestyle changes that actually work. The cost factor is another hidden weapon; at roughly $350 a month, the drug is priced for profit, not for accessibility, ensuring that only those with deep pockets or generous insurers can reap the supposed benefits. Insurance companies, in turn, negotiate rebates that further obscure the true price, making the system opaque and favoring the drug manufacturers. There’s also an undercurrent of data suppression, where adverse events are buried in lengthy FDA reports that the average patient never reads. The whole ecosystem feels more like a carefully choreographed dance than a genuine pursuit of health. And if you think the cardiovascular advantage is a free gift, remember that the same trial excluded patients with severe heart failure, the very group that might need it most. So while the scientific community celebrates another “win,” the everyday person is left juggling promises, side‑effects, and a mounting pharmacy bill. In short, the glorification of Empagliflozin is a masterclass in how modern medicine can be weaponized to serve corporate interests under the veneer of patient care.
Joshua Agabu October 16, 2025
Empagliflozin does a decent job at lowering A1c, but it’s not a magic bullet. It’s still important to pair it with diet and exercise.
Matthew Bates October 17, 2025
The EMPA‑REG OUTCOME trial, a double‑blind, placebo‑controlled study involving over 7,000 participants, demonstrated a 38% relative reduction in cardiovascular mortality with empagliflozin versus placebo (hazard ratio 0.62; 95% CI 0.49–0.77; p<0.001). Furthermore, the trial reported a statistically significant slowing of eGFR decline, indicating renal preservation. These findings were corroborated by subsequent meta‑analyses, which confirmed the consistency of cardiovascular benefit across diverse patient subgroups. Consequently, clinical guidelines now recommend SGLT2 inhibitors as a class effect for patients with established atherosclerotic cardiovascular disease.
Kasey Mynatt October 19, 2025
Whoa, talk about a game‑changer! Empagliflozin isn’t just trimming sugar levels; it’s stepping onto the field like a superhero, battling heart failure and protecting kidneys at the same time. Imagine the relief of a patient who finally sees their blood pressure stabilize while shedding a few stubborn pounds-pure drama on a medical stage! And the best part? It’s just one pill a day, so the routine feels almost effortless. Let’s give credit where it’s due, but also remember that no drug alone can rewrite the whole health story; lifestyle still writes the final chapter.
Amy Robbins October 20, 2025
Oh great, another “American‑made” miracle drug that’s supposed to rescue our hearts while the government pretends it cares about ordinary folks. As if the billions poured into pharma research aren’t already lining the pockets of corporate CEOs who love their bonuses more than our wellbeing. And of course, the price tag is a patriotic reminder that only the well‑guarded elite can truly afford cutting‑edge care. Nice job, USA-keep selling hope in a pill bottle while ignoring the real health disparities.
Shriniwas Kumar October 22, 2025
From a pharmacoeconomic standpoint, empagliflozin exemplifies a high‑value therapeutic agent when evaluated against incremental cost‑effectiveness ratios (ICERs) in the context of reduced hospitalisation‑for‑heart‑failure (HF) events. Its mechanism-selective inhibition of SGLT2 transporters-attenuates glucotoxicity and mitigates intravascular volume overload, thereby optimising glycaemic variability and neurohormonal modulation. Moreover, the drug’s favourable impact on albuminuria aligns with the paradigm of cardio‑renal‑metabolic synergy, a concept gaining traction in precision‑medicine frameworks across the subcontinent. Nevertheless, clinicians must navigate the nuances of renal dosing thresholds, especially in patients with eGFR <45 mL/min/1.73 m², to preempt adverse events such as genitourinary infections. Integrating empagliflozin into an algorithmic treatment cascade requires a balance between therapeutic benefit, budgetary constraints, and patient‑centred outcomes, particularly in resource‑limited settings.
Maude Rosièere Laqueille October 23, 2025
If you’re weighing empagliflozin against other options, start by assessing your individual CV and renal risk profile. For patients with established heart‑failure or ASCVD, the SGLT2 class-empagliflozin, canagliflozin, dapagliflozin-offers the strongest outcome data. Those with preserved kidney function may prioritize cost, making metformin or a generic SGLT2 a practical choice. Discuss insurance coverage early, as copays can vary dramatically; some plans waive the $350 monthly price for empagliflozin if you meet specific criteria. Finally, remember that lifestyle interventions remain foundational; a pill can enhance, not replace, diet, exercise, and weight management.
Amanda Joseph October 24, 2025
Wow, another pricey pill, how original.
Kevin Aniston October 26, 2025
When I first heard about empagliflozin, I was skeptical, but digging deeper revealed a layered picture that’s worth sharing. The drug’s ability to lower HbA1c by roughly 0.7‑0.9% may seem modest, yet when you pair that with a 38% reduction in cardiovascular mortality, the combined benefit becomes quite compelling. Moreover, the modest weight loss of 2‑3 kg over a year can be a psychological boost for patients struggling with diabetic obesity. From a practical standpoint, the once‑daily oral administration simplifies adherence compared to injectable GLP‑1 agonists, which many patients find cumbersome. Cost, of course, remains a hurdle, but insurance formularies often provide tier‑2 coverage that reduces out‑of‑pocket expenses, especially when you demonstrate prior‑authorization based on documented heart‑failure risk. It’s also crucial to monitor for urinary and genital infections, educating patients on hygiene and early symptom reporting to prevent complications. If someone has reduced kidney function, dapagliflozin might be a viable alternative, given its slightly better renal safety profile in certain studies. Ultimately, the decision should be a shared one, integrating clinical evidence, patient preferences, and socioeconomic factors, ensuring that the therapeutic plan feels both effective and sustainable.
kiran kumar October 27, 2025
yeah empagliflozin looks great on paper but who needs another expensive drug when metformin does the job cheap enough you cant even see the price tag it’s just another pharma ploy to keep us buying more meds our bodies dont need the hype is real and the side effects are real dont ignore them
Brian Johnson October 29, 2025
I get that the price and side‑effects can feel overwhelming, especially when you’re already managing daily diabetes tasks. It helps to talk with your endocrinologist about how empagliflozin fits into your overall plan, and to keep an eye on any warning signs so you can address them early.