One glass of grapefruit juice might seem like a healthy start to your day-rich in vitamin C, low in calories, and full of antioxidants. But if you’re taking an immunosuppressant after a transplant, that glass could be hiding a serious danger. This isn’t a myth. It’s not a warning you can ignore. And it’s not something that only happens if you eat a whole fruit. Even a small amount can push your medication levels into a toxic range.
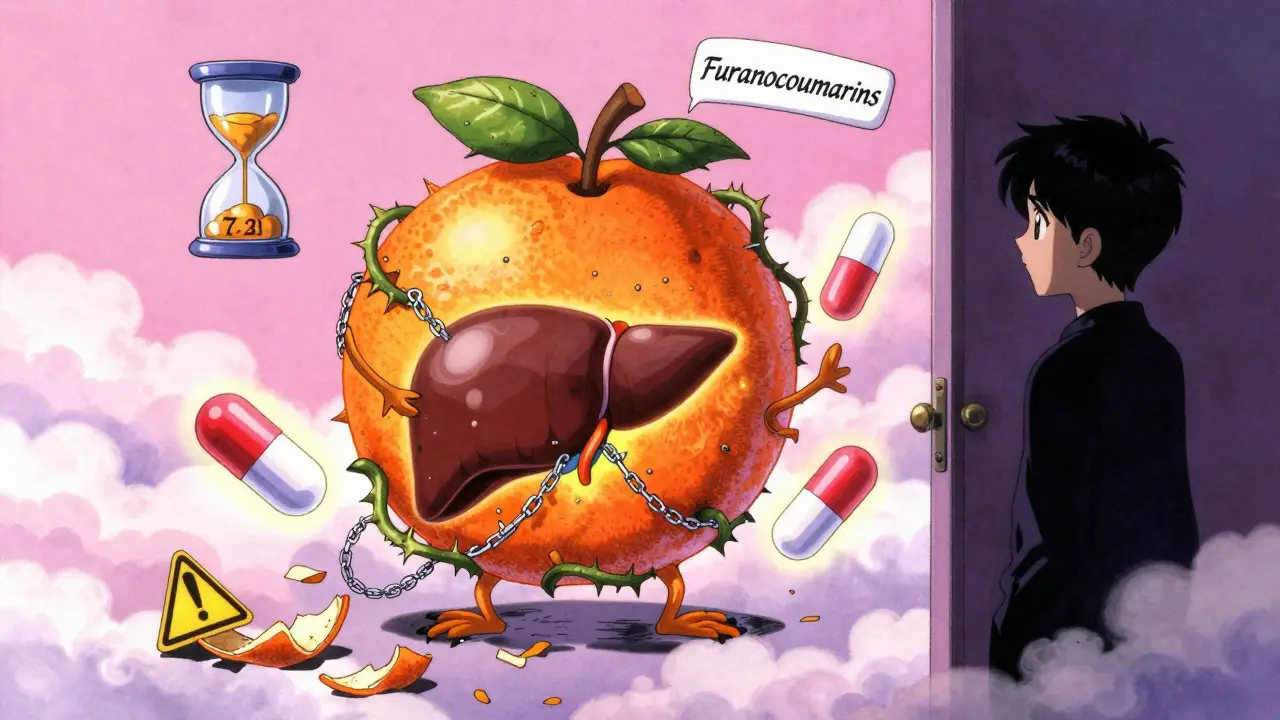
Why Grapefruit Changes How Your Medication Works
The problem isn’t grapefruit itself. It’s what’s inside it: compounds called furanocoumarins, mainly 6',7'-dihydroxybergamottin and bergamottin. These chemicals don’t just sit in your stomach. They go straight to your intestines and shut down an enzyme called CYP3A4. This enzyme is your body’s natural filter for many drugs, including key immunosuppressants like cyclosporine, tacrolimus, and sirolimus. Normally, CYP3A4 breaks down about half of these medications before they even enter your bloodstream. That keeps your blood levels steady and safe. But when grapefruit blocks this enzyme, up to 300% more of the drug gets absorbed. Your body can’t process it fast enough. The result? Toxic levels build up quickly. This isn’t a temporary spike. The damage lasts. Studies show that just one 8-ounce glass of grapefruit juice can inhibit CYP3A4 for up to 72 hours. That means even if you drink grapefruit juice on Monday, your body is still vulnerable on Thursday. There’s no safe window. No "just one time" exception.Which Immunosuppressants Are at Risk?
Not all immunosuppressants react the same way. But the ones that do are critical to your survival after a transplant. The big three are:- Cyclosporine (Sandimmune, Neoral): Grapefruit can raise blood levels by 50% to 100%. Normal therapeutic range: 100-400 ng/mL. Toxic levels start above 500 ng/mL.
- Tacrolimus (Prograf, Envarsus XR, Astagraf XL): Levels can jump 30% to 50%. Normal range: 5-15 ng/mL. Toxic above 20 ng/mL.
- Sirolimus (Rapamune): This one’s especially dangerous. Grapefruit can double or even triple blood concentrations. Normal range: 4-12 ng/mL. Toxic levels can trigger organ damage.
What Happens When Levels Go Too High?
High levels of these drugs don’t just make you feel off. They cause real, life-threatening damage.- Kidney injury: Cyclosporine and tacrolimus are toxic to the kidneys. Too much can cause acute kidney failure, requiring dialysis.
- High blood pressure: These drugs constrict blood vessels. Elevated levels spike blood pressure fast, increasing stroke risk.
- Neurological problems: Tremors, headaches, seizures, and confusion are common signs of toxicity.
- Electrolyte imbalances: High potassium (hyperkalemia) can trigger dangerous heart rhythms.
- Increased infection risk: Over-suppressing your immune system leaves you open to pneumonia, sepsis, and other serious infections.
What About Other Citrus Fruits?
You might think, "Well, I’ll just switch to oranges." But not all citrus is safe.- Regular oranges, tangerines, and lemons: These are generally fine. They don’t contain significant amounts of furanocoumarins.
- Seville oranges: These are used in marmalade and are just as dangerous as grapefruit. Don’t assume "orange" means safe.
- Pomelo: This large citrus fruit is a close relative of grapefruit and contains the same harmful compounds.
- Grapefruit extracts, supplements, or flavored products: Even if it’s labeled "natural flavor," it could contain enough furanocoumarins to cause harm.
How Long Do You Need to Avoid It?
The 72-hour rule isn’t a suggestion. It’s a medical requirement. Because furanocoumarins permanently disable CYP3A4 enzymes in your gut, your body needs time to grow new ones. That takes about three days. So if you accidentally eat grapefruit on Monday, you’re still at risk on Thursday-even if you haven’t had any since. Transplant centers like the University of Pittsburgh Medical Center require patients to avoid grapefruit for at least 72 hours before starting a new medication or adjusting a dose. If exposure is suspected, they immediately check blood levels and reduce the drug dose by 25-50% until results come back.What Should You Do Instead?
You don’t have to give up citrus entirely. Here’s what’s safe:- Oranges (navel, blood, Valencia)
- Tangerines and clementines
- Lemons and limes
- Green apples, berries, pears
- Watermelon, pineapple, and papaya
Why Do So Many People Still Eat It?
It’s not because they’re careless. It’s because they don’t know. A 2023 survey by the British Liver Trust found that 68% of transplant patients didn’t realize how dangerous grapefruit was. Many thought the warning only applied to alcohol or other drugs. Others believed it was an old myth that didn’t apply anymore. Pharmacists at Mayo Clinic report that 15-20% of unexpected immunosuppressant toxicity cases in 2021-2022 were linked to patients hiding grapefruit use. Some didn’t think it mattered. Others didn’t realize it was a problem. This isn’t about blame. It’s about education. The FDA has required grapefruit warnings on medication labels since 2010. But if you’re not reading the leaflet in your pill bottle-or if you got your prescription from a clinic that didn’t explain it-you might not know.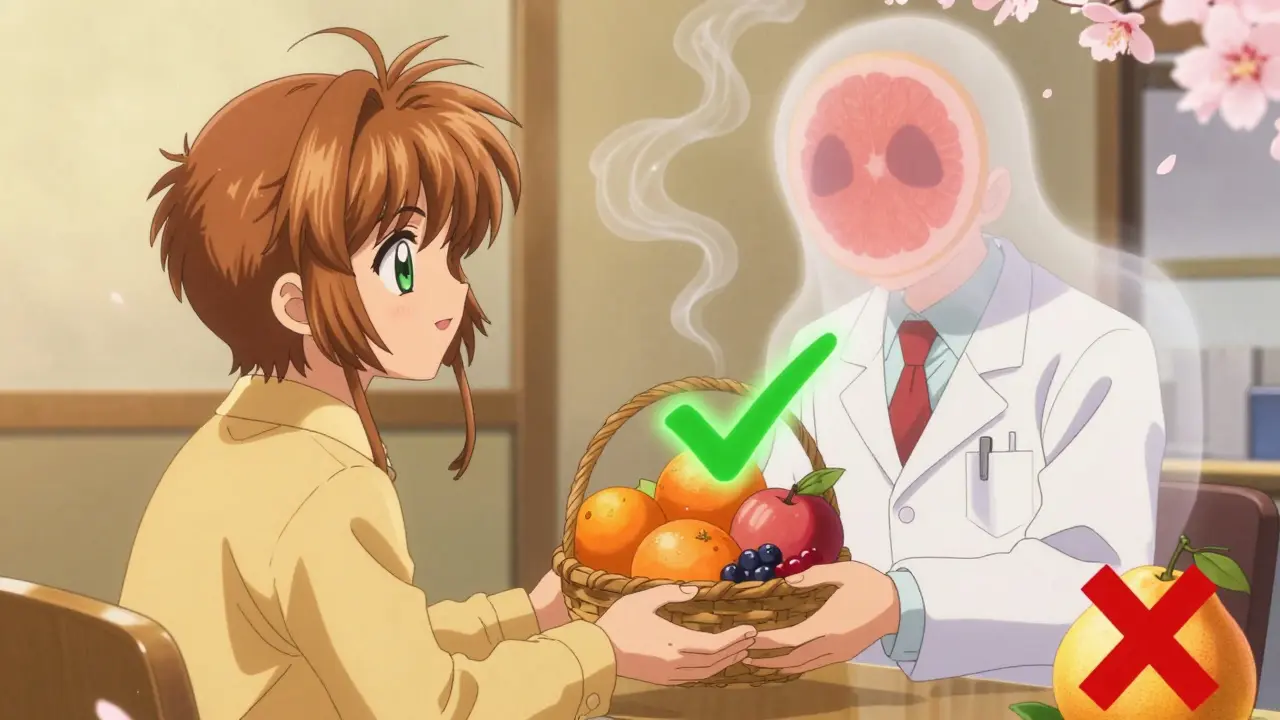
What’s Being Done to Fix This?
The medical community is stepping up. Johns Hopkins launched a mobile app in January 2023 that scans your medication barcode and instantly alerts you if grapefruit is dangerous with your drug. The American Society of Health-System Pharmacists added everolimus (Zortress) to their high-risk list in March 2023. Pharmaceutical companies are trying too. Astellas Pharma developed Envarsus XR, a slow-release version of tacrolimus that reduces-but doesn’t eliminate-the grapefruit interaction. Still, the warning remains: avoid grapefruit entirely. The bigger issue? Aging transplant recipients. About 40% of kidney transplant patients are over 65. Many of them eat grapefruit for its heart-healthy benefits. The United Network for Organ Sharing predicts grapefruit-related toxicity cases will rise 15% over the next decade simply because more older people are living longer after transplants.What to Do Right Now
If you’re on an immunosuppressant:- Check your medication bottle. Look for "grapefruit" in the warning section.
- Ask your pharmacist: "Is grapefruit dangerous with this drug?" Don’t assume they’ll tell you unless you ask.
- Remove all grapefruit, pomelo, and Seville orange products from your kitchen.
- Teach your family. Someone might bring you a smoothie without realizing it’s risky.
- Set a phone reminder: "No grapefruit-ever."
- Call your transplant team immediately.
- Don’t wait for symptoms. Toxicity can happen before you feel anything.
- Expect a blood test within 24-48 hours.
Final Thought: It’s Not Just About Food
Grapefruit is just one example. There are over 85 medications that interact with it-statins, blood pressure drugs, anti-anxiety meds. But for transplant patients, the stakes are higher. Your body doesn’t have a backup plan. One wrong bite, one sip, one forgotten warning-and your immune system could turn on your new organ. Don’t gamble with it. Don’t assume it’s "not that bad." Don’t think "I’ll just have it once." Your health isn’t worth the risk.Can I have orange juice instead of grapefruit juice while on immunosuppressants?
Yes, regular orange juice (navel, Valencia, blood oranges) is generally safe. Unlike grapefruit, it doesn’t contain furanocoumarins-the compounds that block the CYP3A4 enzyme. But avoid Seville oranges, which are used in marmalade and behave like grapefruit. Always check labels for "Seville orange" or "pomelo" in ingredients.
How long after eating grapefruit should I wait before taking my immunosuppressant?
You need to wait 72 hours (three full days). The enzyme-blocking effect from grapefruit lasts that long because furanocoumarins permanently disable intestinal CYP3A4 enzymes. Your body needs time to produce new ones. Even if you haven’t had grapefruit in 24 hours, you’re still at risk. The safest approach is to avoid it completely while on these medications.
What if I accidentally ate grapefruit? Should I skip my next dose?
Do not skip your dose on your own. Instead, contact your transplant team immediately. Skipping your medication can cause your immune system to attack your new organ. The correct response is to get a blood test to check your drug levels. Your doctor may lower your dose temporarily based on the results, but only they should make that decision.
Are all forms of grapefruit dangerous-even extracts or supplements?
Yes. Grapefruit extracts, essential oils, powders, and even flavorings in supplements or protein shakes can contain enough furanocoumarins to cause a dangerous interaction. Don’t assume "natural flavor" is safe. If it’s derived from grapefruit, pomelo, or Seville orange, avoid it. Always read ingredient lists carefully.
Why do some people say grapefruit is healthy but still warn against it with meds?
Grapefruit is nutritionally valuable-it’s high in vitamin C, fiber, and antioxidants. The American Heart Association even gives it a heart-check mark. But health benefits don’t cancel out drug risks. For transplant patients, the danger of toxic medication levels far outweighs the nutritional benefit. It’s not about the fruit being bad-it’s about how it interferes with your body’s ability to process life-saving drugs.
Is there any way to reverse the grapefruit interaction once it happens?
There’s no proven way to reverse the effect once furanocoumarins have blocked CYP3A4. Some early research suggests activated charcoal might reduce absorption if taken within an hour of grapefruit consumption, but this isn’t standard practice and shouldn’t be relied on. The only reliable solution is prevention. Avoid grapefruit entirely while on immunosuppressants.








Raushan Richardson December 28, 2025
Just had my first transplant checkup last week, and my nurse handed me a printed list of "DO NOT EAT" foods. Grapefruit was at the top. I cried. Not because I’m sad about giving it up-but because I didn’t know. I thought it was just a myth people told to scare you. Turns out, I’ve been drinking grapefruit juice every morning for three years. My doctor said I’m lucky I didn’t crash my kidneys yet. Now I’m on orange juice and berries. Still sad, but alive.
Thank you for this post. Seriously. Someone needed to say it like it is.
John Barron December 29, 2025
While your article is factually accurate, it lacks the requisite depth of pharmacokinetic nuance. The inhibition of CYP3A4 by furanocoumarins is not merely enzymatic blockade-it is an irreversible, time-dependent inactivation requiring de novo synthesis of intestinal cytochrome P450 isoforms. Moreover, the 72-hour window is conservative; in elderly patients with reduced hepatic regeneration capacity, enzyme recovery may extend to 96–120 hours. Furthermore, the pharmacogenetic variability of CYP3A5 expression-particularly in African descent populations-may modulate the severity of interaction. A 2022 study in the Journal of Clinical Pharmacology demonstrated that CYP3A5*3 homozygotes exhibit 40% higher tacrolimus AUC following grapefruit exposure than non-carriers. Your omission of this genetic dimension renders your guidance incomplete.
Liz MENDOZA December 30, 2025
My mom is a kidney transplant recipient, and this post made me cry. She used to love grapefruit for breakfast. I didn’t realize how dangerous it was until she got hospitalized last year. We’ve since cleaned out her fridge, bought her a fruit basket with oranges and pears, and even started a little weekly ritual: we make smoothies together using safe fruits. She says it’s the new normal. I say it’s a gift. Thank you for making this so clear. To anyone reading this: if you’re caring for someone on immunosuppressants, don’t assume they know. Ask. Check. Help.
And if you’re on meds-please, for your family’s sake, don’t risk it.
Caitlin Foster January 1, 2026
So let me get this straight… I can’t have grapefruit juice, but I can have 17 different kinds of protein powder that say "natural flavor"? 😭
Also, why is this still a thing in 2025? I’ve had this conversation with my pharmacist THREE times. She rolls her eyes. I roll mine. We both know I’m gonna forget. Again. 😅
Todd Scott January 1, 2026
As someone who lived in Nigeria before moving to the U.S., I want to share a cultural perspective. In parts of West Africa, citrus fruits like pomelo are common in traditional remedies for hypertension and diabetes. Many elders believe "natural means safe." When I first heard about grapefruit interactions, I thought it was an American overreaction. But after my cousin-on tacrolimus after a liver transplant-ended up in ICU from a homemade pomelo smoothie, I realized: cultural familiarity doesn’t override biochemistry. I now carry printed handouts in both English and Yoruba for my family. Knowledge isn’t enough-it must be communicated in the language people understand. This isn’t just a medical issue. It’s a public health literacy crisis.
Andrew Gurung January 3, 2026
Ugh. Another "do this or die" post. 😒
Look, if you’re dumb enough to drink grapefruit juice while on life-saving meds, you probably also think "organic" means "immune to science." I’ve seen it before. People think they’re "natural healers"-then wonder why their new kidney is failing. It’s not the grapefruit’s fault. It’s yours. You didn’t read the label. You didn’t ask. You thought you were too cool for warnings.
Next time, maybe take responsibility instead of blaming the fruit. 🙄
Paula Alencar January 4, 2026
The gravity of this issue cannot be overstated. The pharmacodynamic consequences of CYP3A4 inhibition extend beyond mere pharmacokinetic alteration-they represent a fundamental breach in the homeostatic equilibrium of post-transplant immunological tolerance. The irreversible nature of furanocoumarin-induced enzyme inactivation necessitates not merely avoidance, but a paradigmatic reorientation of dietary behavior. Patients must be educated not as passive recipients of instructions, but as active agents in their own survival. The 72-hour window is not arbitrary; it is the temporal threshold of enzymatic regeneration. Failure to adhere constitutes not negligence, but existential risk. I implore every healthcare provider: do not rely on printed inserts. Do not assume patient comprehension. Conduct mandatory, documented, multilingual counseling sessions. Lives are not abstract statistics. They are mothers, fathers, children-waiting for someone to speak plainly.
Nikki Thames January 4, 2026
It’s fascinating how we anthropomorphize food. Grapefruit didn’t "betray" you. It’s not evil. It’s just a fruit with a biochemical quirk. The real problem is our collective refusal to engage with pharmacology as a science. We want our vitamins and our safety, but we refuse to learn the mechanics. Why? Because it’s inconvenient. Because it requires effort. Because we’d rather believe in myths than memorize a single enzyme name. This isn’t about grapefruit. It’s about human denial. And until we face that, we’ll keep burying transplants under citrus peels.
Chris Garcia January 6, 2026
In my village in Nigeria, we say: "The hand that feeds you can also poison you." Grapefruit is not the enemy-it is a mirror. It reflects our ignorance, our haste, our trust in taste over science. My uncle, a diabetic, once drank grapefruit juice with his pills because "it tasted better." He lost his kidney. We buried him with a single orange beside his casket. No grapefruit. No pomelo. No lies. Just truth, wrapped in peel. I now teach this to every young person I meet: your body is a temple, but even temples need blueprints. Read them. Ask. Learn. Then eat. Not because you’re scared-but because you’re wise.
James Bowers January 7, 2026
Incorrect. The 72-hour window is not universally applicable. Pharmacokinetic studies demonstrate significant interindividual variability in CYP3A4 recovery rates. The assertion that "no safe window exists" is an oversimplification that may induce unnecessary dietary anxiety. A 2021 meta-analysis in Transplantation Proceedings suggests that in patients with high baseline CYP3A4 activity, partial enzyme recovery may occur as early as 48 hours. Therefore, blanket prohibitions without individualized risk assessment are clinically inappropriate.
Will Neitzer January 8, 2026
Thank you for this comprehensive, meticulously referenced, and urgently needed resource. As a transplant coordinator, I’ve witnessed too many preventable hospitalizations due to grapefruit ingestion. I’ve seen patients cry because they thought "a little bit wouldn’t hurt." I’ve seen families blame the doctor because they weren’t told clearly enough. This post does what clinics often fail to do: it speaks with clarity, compassion, and scientific rigor. I’m sharing it with every new patient and their caregivers. Please, if you’re reading this and you’re on immunosuppressants-don’t wait for a warning label. Ask your pharmacist. Write it down. Tell your kids. This isn’t about fear. It’s about love. And love means being responsible. Thank you for reminding us.
Janice Holmes January 9, 2026
THEY SAID IT WAS "JUST A WARNING." THEY DIDN’T SAY IT COULD KILL YOU.
My husband’s creatinine spiked to 5.8 after one glass. One. Glass. We were in the ER at 3 a.m. He had to go on dialysis for 10 days. His new kidney? Still there. But barely. The doctors said if we’d waited another 12 hours, he’d have lost it. Forever.
I threw out every grapefruit, every juice, every smoothie with "natural flavor." I bought him a fruit calendar. I set alarms. I screamed at him every time he reached for a juice box.
Don’t be the person who says "I didn’t know."
Because now I know.
And I’ll never let anyone forget it.