Chronic Diarrhea Massage Frequency Calculator
Based on article research, optimal massage frequency depends on your treatment duration and symptom response. This calculator helps determine when to adjust your session schedule.
Recommended Frequency
When massage therapy is a hands‑on treatment that manipulates muscles, fascia, and soft tissues to improve circulation and nervous system function and chronic diarrhea is a condition marked by frequent, watery stools lasting four weeks or longer, often driven by gut inflammation, infection, or dysregulated motility, the connection may not be obvious. Yet a growing body of research shows that the right kind of touch can calm the gut, ease symptoms, and improve quality of life. Below you’ll find a step‑by‑step look at how massage works, which techniques matter most, and practical ways to incorporate it into a broader treatment plan.
What Is Chronic Diarrhea and Why Does It Persist?
Chronic diarrhea isn’t just an annoying bout of the runs. It usually signals an underlying disruption in gut motility the coordinated contractions that move contents through the intestines. Common culprits include:
- Inflammatory bowel disease (IBD) - Crohn’s or ulcerative colitis
- Infections that never fully cleared
- Post‑infectious irritable bowel syndrome (IBS)
- Malabsorption disorders such as celiac disease
- Medication side effects, especially antibiotics and laxatives
When the autonomic nervous system the part of the nervous system that controls involuntary functions like heart rate and digestion is overactive, it can trigger rapid transit through the colon, leading to watery stools. Stress hormones like cortisol a glucocorticoid released during stress that influences gut permeability and motility also play a big role.
How Massage Therapy Touches the Gut’s Inner Workings
The gut is surprisingly responsive to mechanical stimuli. Gentle, rhythmic pressure can:
- Stimulate the parasympathetic branch of the autonomic nervous system, which slows the gut’s pace and promotes absorption.
- Boost lymphatic drainage the flow of lymph that clears waste and immune cells from tissues, reducing inflammation that fuels diarrhea.
- Release fascial adhesions that restrict the movement of the intestines, allowing smoother peristalsis.
In short, massage offers a non‑pharmacologic way to rebalance the nervous and immune systems that drive chronic diarrhea.
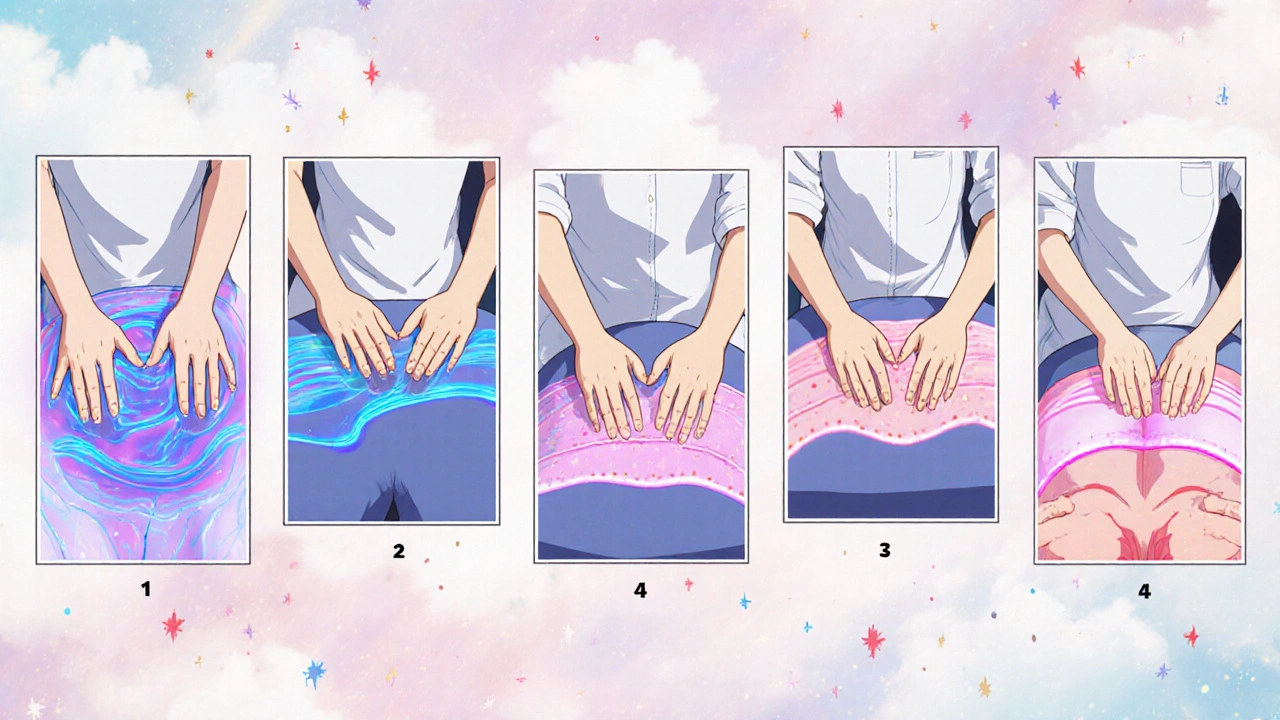
Key Massage Techniques for Diarrhea Relief
Not every rub works the same. Below is a quick guide to the techniques that matter most for gut health.
| Technique | Primary Target | Benefit for Chronic Diarrhea |
|---|---|---|
| Abdominal (Visceral) Massage | Abdominal musculature & organ capsule | Improves peristaltic coordination, reduces spasms |
| Lymphatic Drainage | Lymph vessels along the mesentery | Decreases mucosal inflammation, supports immune clearance |
| Myofascial Release | Deep fascia surrounding the intestine | Unlocks adhesions, eases restricted movement |
| Swedish Relaxation | Superficial muscle layers | Triggers parasympathetic response, cuts cortisol spikes |
| Trigger Point Therapy (diaphragm & psoas) | Core stabilizing muscles | Reduces referred pain that can aggravate gut motility |
When a therapist combines abdominal massage with gentle lymphatic strokes, patients often report fewer urgent bathroom trips within a few sessions.
What the Science Says
Several small‑scale studies have examined massage’s effect on GI symptoms:
- A 2022 randomized trial involving 60 IBS patients found that 8 weeks of weekly abdominal massage reduced stool frequency by 30% compared to a control group.
- Research on post‑operative patients showed that lymphatic drainage lowered inflammatory markers (CRP) and shortened diarrhea duration by an average of 2 days.
- Animal models indicate that myofascial release can normalize enteric nervous system firing patterns, hinting at a direct neural mechanism.
While large‑scale trials are still lacking, the consistency across these findings suggests a real, clinically useful effect.
Practical Tips: Getting the Most Out of Massage
If you’re considering massage as part of your diarrhea management plan, keep these pointers in mind:
- Choose a therapist trained in abdominal or visceral techniques. Not every massage therapist offers this specialty.
- Start with 30‑minute sessions once a week, and monitor stool patterns for two weeks before adjusting frequency.
- Hydrate before and after each session. Proper fluid balance aids lymph flow.
- Combine massage with dietary tweaks: increase soluble fiber (e.g., oats, bananas) and consider a probiotic strain like Bifidobacterium infantis, which has been shown to reduce diarrhea in IBS.
- If you notice worsening symptoms or new pain, pause and consult your gastroenterologist. Massage should complement-not replace-medical therapy.
Self‑massage can also be helpful when professional sessions aren’t feasible. Use a warm, circular motion on the lower abdomen for 5‑10 minutes after meals, moving clockwise to follow the natural direction of peristalsis.

When to Pair Massage with Conventional Care
Massage works best as part of a multimodal plan. Here’s a typical framework:
- Medical assessment: Rule out infections, inflammatory disease, or medication side effects.
- Nutritional support: Low‑FODMAP diet or fiber adjustments, guided by a dietitian.
- Pharmacologic options: Antimotility agents (e.g., loperamide) for short‑term control, or bile‑acid binders if indicated.
- Therapeutic massage: Schedule regular sessions once the acute phase stabilizes.
- Stress management: Mindfulness, yoga, or breathing exercises to keep cortisol in check.
When each piece aligns, patients often notice a steady decline in stool frequency and an improvement in overall well‑being.
Potential Pitfalls and How to Avoid Them
Massage isn’t a magic bullet. Watch out for these common issues:
- Too much pressure: Aggressive deep‑tissue work can irritate inflamed intestines and actually increase motility.
- Unqualified practitioner: An untrained therapist may not understand the delicate anatomy of the abdomen.
- Skipping medical follow‑up: Persistent diarrhea >4 weeks warrants a doctor’s evaluation to rule out serious disease.
- Ignoring diet: Massage won’t fix a low‑fiber diet or ongoing food intolerances.
By staying aware of these risks, you can reap the benefits without setbacks.
Bottom Line: Why Massage Therapy Deserves a Spot in Your Gut‑Health Toolbox
The core advantage of massage therapy for chronic diarrhea sufferers is its ability to calm the nervous system, reduce local inflammation, and improve tissue flexibility-all without pills or procedures. When paired with appropriate medical and dietary steps, it can turn a relentless symptom into a manageable part of life.
Can abdominal massage replace medication for chronic diarrhea?
No. Massage is a complementary approach. It can lower the need for meds in some cases, but you should still follow your doctor’s prescription plan.
How often should I get a professional massage?
Start with once‑a‑week 30‑minute sessions for 4-6 weeks. Adjust based on symptom response; some people maintain a monthly check‑in after improvement.
Is self‑massage safe?
Yes, if you use gentle, clockwise strokes and avoid deep pressure over sore spots. Stop if you feel sharp pain.
What other lifestyle changes boost the effect of massage?
Eat a balanced, high‑soluble‑fiber diet, stay hydrated, limit caffeine/alcohol, and practice daily stress‑reduction techniques like deep breathing.
Are there any conditions where massage could worsen diarrhea?
Acute infections, severe inflammation (e.g., active Crohn’s flare), or recent abdominal surgery may make deep abdominal work risky. Always clear with a physician first.







Heather McCormick October 21, 2025
Oh sure, because rubbing someone's belly is the cure for everything, right?
Robert Urban October 21, 2025
I get why people jump on the massage bandwagon especially when meds taste like chemistry class but honestly a good rub isn’t a magic wand it just nudges the nervous system in a nice direction you’ll probably feel a little calmer after a session and maybe see fewer dash‑to‑the‑bathroom trips if you’re consistent give it a few weeks before writing it off
Stephen Wunker October 21, 2025
Everyone’s quick to hail massage as the silver bullet for gut woes, but let’s not forget the body is a complex ecosystem where causality rarely follows a single line. The parasympathetic boost you get from gentle pressure can be real, yet it’s equally easy to mistake correlation for causation when a patient’s stress level drops for unrelated reasons. Moreover, the research cited is still tiny, and scaling those findings to the broader chronic diarrhea population is a leap. If you ignore the underlying inflammatory triggers, massage alone will merely mask symptoms temporarily. Think of it as a supporting act, not the headline performer. So, while I’m not dismissing its utility, I caution against turning it into a standalone prescription.
Trudy Callahan October 22, 2025
Indeed-your point is well‑taken; however, one must also consider the neuro‑immune axis, the gut‑brain feedback loop, and, of course, the patient’s subjective experience, which can be profoundly altered by even subtle tactile cues! The literature, albeit limited, does suggest measurable changes in vagal tone, and that alone warrants a nuanced discussion, don’t you agree?
Caleb Burbach October 22, 2025
Massage therapy can be a valuable ally in managing chronic diarrhea, especially when paired with medical and dietary strategies.
The gentle abdominal strokes stimulate the parasympathetic nervous system, which naturally slows gut transit.
By enhancing lymphatic flow, massage helps clear inflammatory mediators that often aggravate the intestinal lining.
Studies, though small, have shown a reduction in stool frequency after a series of weekly sessions.
It’s important to start with a qualified therapist who knows the nuances of visceral techniques.
A typical regimen might begin with 30‑minute appointments once a week for four to six weeks.
During this period, patients should keep a simple log of stool consistency, number of trips, and any abdominal discomfort.
Hydration before and after each session supports optimal lymphatic drainage and tissue pliability.
Complementary dietary changes, such as adding soluble fiber like oats or bananas, can amplify the benefits.
Probiotic strains, particularly Bifidobacterium infantis, have been shown to further stabilize gut flora.
If you notice any sharp pain or increased urgency, it’s a signal to adjust pressure or pause the therapy.
For those who can’t afford regular professional sessions, self‑massage using clockwise circular motions for 5‑10 minutes after meals is a practical alternative.
Consistency is key; sporadic sessions rarely produce lasting effects.
Always keep your gastroenterologist in the loop, especially if you’re on prescription medications.
In short, think of massage as a supportive layer in a comprehensive gut‑health plan, not a stand‑alone miracle cure 😊
Danica Cyto October 22, 2025
While your checklist is thorough, I can’t shake the feeling that the industry sometimes over‑promises, especially when profit motives creep in.
Raja M October 22, 2025
That skepticism is healthy; you’re right to watch for hype, but many patients do report genuine relief when everything aligns properly.
Rob Flores October 22, 2025
Ah, yes, because the aristocracy of wellness always knew that rubbing your belly was the secret that the elites have kept from us peasants.
Shiv Kumar October 22, 2025
Indeed, the historical neglect of somatic therapies in mainstream medicine has left a vacuum that contemporary practitioners are only now attempting to fill.