Most people never look at the medication guide that comes with their prescription. They grab the pills, toss the paper in the drawer, and hope for the best. But that guide? It’s not just filler. It’s your first line of defense against overdose - especially if you’re taking opioids, benzodiazepines, or other high-risk medications.
Where to Find the Overdose Warnings
Every FDA-approved prescription medication in the U.S. comes with a Medication Guide - a printed sheet that’s required by law to explain serious risks in plain language. It’s not the same as the package insert doctors read. This one’s meant for you.Open your pill bottle. Look for a small, folded paper, usually white or light yellow, tucked under the cap or stuck to the side of the box. It’s often labeled “Medication Guide” in bold at the top. Don’t skip it. The most important section for overdose prevention is called Overdosage. That’s where you’ll find the exact amount that could be dangerous, and what to do if someone takes too much.
Understanding the Warning Signs
The guide doesn’t just say “don’t overdose.” It tells you what happens when you do. For opioids like oxycodone or fentanyl, the warning will list symptoms like:- Slow, shallow, or stopped breathing
- Unconsciousness or inability to wake up
- Pinpoint pupils
- Lips or fingernails turning blue or purple
For benzodiazepines like alprazolam or diazepam, you might see: “Excessive sedation, confusion, loss of coordination, or coma may occur with overdose.”
These aren’t vague suggestions. They’re clinical facts based on real overdose cases. If you or someone you know shows even one of these signs after taking your medication, it’s not a “bad reaction” - it’s an emergency. And the guide will tell you exactly why.
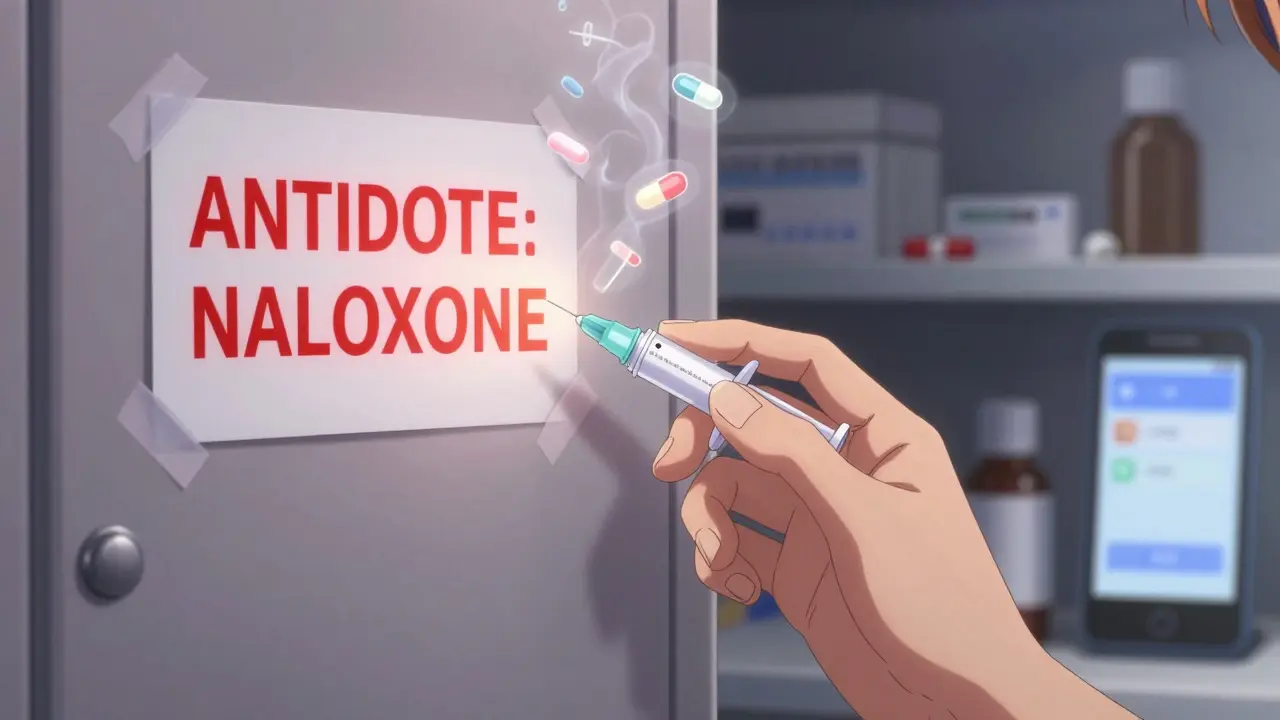
Locating the Antidote Information
This is the part most people miss. Under the Overdosage section, you’ll often find a line like: “Naloxone may be used as an antidote.” Or: “Flumazenil is indicated for reversal of benzodiazepine overdose.”That’s not just jargon. It’s your lifeline. Naloxone - the opioid antidote - is available over the counter in all 50 states. But if you don’t know your medication has an antidote, you won’t ask for it. You won’t keep it in your medicine cabinet. You won’t know to call 911 and grab it at the same time.
Look for the word “antidote” or “reversal agent.” If it’s listed, write it down. Keep a note on your phone. Tell a family member. If you’re on long-term pain medication, ask your pharmacist: “Is there an antidote for this? Can I get it without a prescription?”
What the Boxed Warning Means
Sometimes, the guide will reference a “Boxed Warning” - the strongest warning the FDA can require. It’s printed in a black border at the top of the full prescribing information (which you can find online). The Medication Guide will summarize it in plain terms.For example, a Boxed Warning for a combination painkiller (like oxycodone and acetaminophen) might say: “Fatal respiratory depression may occur, especially with misuse or when combined with alcohol or benzodiazepines.”
That’s not a suggestion. That’s a red flag. If your guide mentions a Boxed Warning, treat it like a fire alarm. Don’t ignore it. Don’t rationalize it. Don’t assume “it won’t happen to me.” It happens to people who thought the same thing.
Reading Between the Lines: What’s Not Said
Medication guides don’t always spell out everything. For example, they might say “Do not drink alcohol while taking this medication.” But they won’t always say: “Even one drink can slow your breathing enough to cause death.”That’s why you need to cross-reference. If your guide warns about drowsiness or dizziness, assume it’s also warning you about slowed breathing. If it says “may cause sedation,” assume it’s also saying “may cause respiratory depression.”
Also watch for phrases like “use with caution in patients with respiratory disease.” That’s code for: “If you have asthma, sleep apnea, or COPD, this drug can kill you even at normal doses.”

What to Do After You Read It
Reading the guide is only step one. Here’s what to do next:- Keep the guide visible. Tape it to your medicine cabinet or stick it on your fridge. Don’t let it get lost.
- Share it with someone. Give a copy to a roommate, partner, or neighbor. Teach them the overdose signs and where to find naloxone.
- Get naloxone. If your medication has an antidote listed, get it. Pharmacies in Pennsylvania and most U.S. states give it out free or for under $20 without a prescription. Keep one at home, one in your car, one with your bag.
- Set a reminder. Use your phone to set a weekly alert: “Review my meds. Check for overdose warnings.”
- Ask your pharmacist. They’re trained to explain these guides. Ask: “Does this have a specific antidote? Is it safe to take with my other meds?”
Common Mistakes People Make
- Assuming “I’ve been taking this for years, so it’s safe.” - Tolerance changes. Your body’s reaction doesn’t stay the same.
- Thinking “My doctor wouldn’t prescribe something dangerous.” - Doctors aren’t always aware of all interactions. The guide is your backup.
- Believing “I’ll know if I’m overdosing.” - Many people don’t feel anything until it’s too late. Breathing slows silently.
- Waiting to act until someone is unconscious. - The guide says symptoms start before collapse. Act at the first sign.
Why This Matters More Than Ever
In 2025, overdose deaths in the U.S. are still climbing. Fentanyl is now found in pills people think are just painkillers or anxiety meds. Even a single pill can be lethal if you’re not used to it.Medication guides are designed to stop this before it happens. They’re not perfect. But they’re the only official, legal, patient-focused source that tells you: This drug can kill you. Here’s how. Here’s how to stop it.
If you take any medication with sedative effects - opioids, sleep aids, muscle relaxants, anti-anxiety drugs - you owe it to yourself to read that guide. Not once. Not when you first get it. But every time you refill. Because the warnings can change. The antidotes can change. And your life might depend on it.
Do all prescription medications come with a Medication Guide?
No. Only medications the FDA has determined carry serious risks - like opioids, benzodiazepines, certain antidepressants, and blood thinners - are required to include one. If you don’t see a guide, ask your pharmacist. Some high-risk drugs still don’t have them, and you should know why.
Can I get naloxone without a prescription?
Yes. In every U.S. state, naloxone is available over the counter at pharmacies like CVS, Walgreens, and Rite Aid. Many community health centers and harm reduction programs give it out for free. You don’t need ID, insurance, or a doctor’s note. Just ask: “I’d like to get naloxone for overdose reversal.”
What if the guide doesn’t mention an antidote?
If there’s no antidote listed, that doesn’t mean there isn’t one - it just means none has been approved for that specific drug. In those cases, emergency care is critical. Call 911 immediately if you suspect overdose. Do not wait. Even without an antidote, breathing support and hospital care can save lives.
Are overdose warnings different for generics vs. brand-name drugs?
No. Generic drugs must have the same Medication Guide as their brand-name counterpart. The FDA requires identical safety information. So if your brand-name drug has a Boxed Warning for overdose, the generic version does too. Don’t assume generics are safer.
How often should I re-read my Medication Guide?
Every time you refill your prescription. Warnings can be updated based on new data. A drug that was safe last year might now carry a stronger warning. Also, if you start a new medication, add alcohol, or develop a new health condition like sleep apnea, your risk profile changes. Re-read the guide every 6 months, or whenever your treatment changes.








Jeffrey Frye December 23, 2025
bro i read this guide after my cousin OD’d on oxycodone and i swear to god it saved his life. we found the naloxone part, called 911, and grabbed the kit from the glovebox. he was blue, not breathing, and we gave him the shot before the ambulance even got there. i didn’t know meds came with death instructions until i had to use them. now i tape the guides to my fridge. no joke.
bharath vinay December 24, 2025
This is all government propaganda. The FDA doesn’t care if you live or die. They just want you dependent on pills so the pharmaceutical giants keep making billions. Naloxone? It’s a tool to keep addicts alive so they keep buying more drugs. Real solution? Stop taking everything the doctor gives you. Your body doesn’t need chemicals to function.
Usha Sundar December 25, 2025
I just threw mine away. Too much drama.
claire davies December 27, 2025
Oh my goodness, this post made me cry. Not because it’s sad, but because it’s so beautifully practical. I’m from London and I had no idea naloxone was available over the counter everywhere in the US - I thought it was still prescription-only here. I just ordered two kits for my flatmates and one for my mum’s house. She’s on gabapentin and we never talked about it, but now I’m printing out the guide and sticking it next to her tea mugs. We all need these little lifelines. Thank you for writing this like a friend, not a textbook.
Harsh Khandelwal December 29, 2025
Why are we even reading these? The pills are made by the same companies that sold us opioids in the 90s. They want you to think you’re safe if you "follow the guide." But they’re the ones who made the overdose epidemic in the first place. Read the guide? Nah. Burn it and call your lawyer.
Andy Grace December 29, 2025
I’ve been on long-term pain meds for 8 years. I never looked at the guide until last year when my doctor switched me to a generic. Same pill, different paper. Turns out the new one had a Boxed Warning I’d never seen before - about combining with sleep apnea meds. I’d been taking both for years. I almost didn’t catch it. Now I read every guide like it’s a survival manual. Because it is.
Abby Polhill December 30, 2025
As a pharmacist’s assistant, I see this daily. People come in for refills and say, "I didn’t get a guide." I hand them one. They say, "Oh, I threw that away." I’ve stopped being shocked. But I still hand them the paper. Because one day, someone’s gonna need it. And that person might be you.
Austin LeBlanc January 1, 2026
You’re telling people to read the guide like it’s some holy scripture? Bro, your doctor knows more than a pamphlet. And if you’re worried about overdose, don’t take the damn pills. Stop being lazy and take responsibility. Also, why are you keeping naloxone in your car? Are you planning to OD on your commute?
Rachel Cericola January 2, 2026
Let me tell you something - I’m a nurse in rural Ohio, and I’ve seen too many families lose someone because they didn’t know the difference between "drowsy" and "not breathing." The guide isn’t just information - it’s a tool for empowerment. I give every patient a printed copy, I highlight the overdose section in yellow, and I ask them to read it aloud to someone they trust. And yes, I’ve had people roll their eyes. But I’ve also had a 17-year-old girl come back three months later and say, "My brother OD’d last week. I used the guide. I gave him the naloxone. He’s alive." That’s why I keep doing this. Not because it’s easy. Because it matters. If you’re on anything that makes you sleepy - opioids, benzos, muscle relaxants, even some antidepressants - you owe it to your future self to read that paper. Not once. Every refill. Write the antidote on your hand if you have to. It’s not paranoia. It’s preparation.
niharika hardikar January 3, 2026
While the intent of this post is commendable, the underlying assumption that patients are passive recipients of medical information is deeply problematic. The onus of risk mitigation should not rest solely on the individual, especially when systemic factors - such as pharmaceutical lobbying, inadequate physician education, and fragmented healthcare access - are primary drivers of overdose incidence. A Medication Guide, while legally mandated, is a Band-Aid on a hemorrhage. True patient safety requires regulatory reform, not behavioral compliance.