JAK Inhibitor Risk Assessment Tool
Risk Assessment
This tool helps you understand your personal risk of serious infections and blood clots when considering JAK inhibitor therapy. Based on your medical profile, it will show whether JAK inhibitors are appropriate for you, or if you should discuss safer alternatives with your doctor.
Your risk assessment will appear here after calculation.
When you're living with rheumatoid arthritis, psoriatic arthritis, or ulcerative colitis, finding a treatment that actually works can feel like a win. JAK inhibitors - drugs like JAK inhibitors tofacitinib, upadacitinib, and baricitinib - promised just that: faster relief than traditional biologics, with pills instead of injections. But since 2021, the story has changed. The FDA added a black box warning - the strongest possible - for these drugs because of two very real dangers: serious infections and blood clots. If you're considering or already taking one, you need to know what to watch for - not just what your doctor says, but what the data shows.
Why JAK Inhibitors Are Different
JAK inhibitors work inside your cells, blocking signals that cause inflammation. Unlike biologics that target proteins outside cells, these small molecules slip into your immune system’s control room and turn down the volume on cytokines. That’s why they work quickly. But that same mechanism is why they mess with more than just inflammation. JAK enzymes are involved in making blood cells, healing wounds, and even fighting viruses. Inhibit them too much, and you open the door to trouble.The Infection Risk Is Real - And Common
Serious infections are the most reported side effect. In clinical trials and real-world use, about 1 in 20 people on JAK inhibitors develop a serious infection requiring hospitalization. That’s twice the rate seen with TNF inhibitors. The most common? Herpes zoster - shingles. Even if you got the vaccine, it’s not foolproof. One patient on Reddit shared how she got shingles within three months of starting tofacitinib, despite being vaccinated. She ended up in the hospital for five days. Other infections include pneumonia, tuberculosis (TB), and fungal infections like histoplasmosis. Some people don’t even feel sick until it’s too late. A 68-year-old man on baricitinib thought he had the flu. He didn’t realize he had invasive aspergillosis - a rare lung fungus - until his oxygen levels crashed. He survived, but barely. The FDA and EMA now require all patients to be screened for TB before starting. You also need up-to-date vaccines: pneumococcal, flu, and shingles. Live vaccines - like MMR or chickenpox - are a hard no while you’re on these drugs. If you’re due for one, get it at least four weeks before starting treatment.Thrombosis: The Silent Killer You Can’t Ignore
Blood clots - specifically venous thromboembolism (VTE) - are the second big red flag. VTE includes deep vein thrombosis (DVT) and pulmonary embolism (PE). Both can kill. A 2022 analysis of over 126,000 patients found JAK inhibitors increased the odds of a clot by more than 2.3 times. The risk jumps even higher if you’re over 65, obese, smoke, or have had a clot before. One woman on upadacitinib had a DVT in her calf after a long flight. She didn’t have pain at first - just swelling. By the time she went to the ER, the clot had traveled to her lung. Her doctor immediately stopped the drug. She’s now on blood thinners and switched to a different treatment. The data shows JAK2 inhibitors - like tofacitinib and baricitinib - carry the highest clot risk because they interfere with platelet production. Upadacitinib, which is more selective for JAK1, seems to have a lower signal, but it’s still there. The FDA says: if you have any risk factors - obesity, history of clots, recent surgery, or use of estrogen - you shouldn’t start a JAK inhibitor unless there’s no other option.Who Should Avoid These Drugs Altogether?
It’s not just about having one risk factor. It’s about the combination. The European Medicines Agency (EMA) says JAK inhibitors should only be used if:- You’re under 65 and have no history of heart disease or clots
- You don’t smoke
- You don’t have cancer or a history of cancer
- You’ve tried and failed at least one TNF inhibitor or other biologic
Monitoring Is Non-Negotiable
You can’t just take the pill and forget it. Regular blood tests are required. Every 4 to 8 weeks, you need a complete blood count to check for low white cells, red cells, or platelets. Lipid panels are also needed - JAK inhibitors raise cholesterol by 15-20% within weeks. That doesn’t mean you’re doomed, but it means you need to manage it with diet, exercise, or statins. The American College of Rheumatology (ACR) recommends checking for signs of infection every visit: fever, cough, unusual fatigue, skin redness, or pain when urinating. If you develop any of these, stop the drug and call your doctor immediately. Don’t wait. Don’t try to tough it out.What About the Newer JAK Inhibitors?
You might hear that newer drugs like upadacitinib or filgotinib are safer. There’s some truth to that. Upadacitinib is more selective for JAK1, which means less impact on blood cell production. Early data from the JAKARTA2 trial showed only 0.2 clots per 100 patient-years with upadacitinib - compared to 0.9 with tofacitinib. That’s promising. But here’s the catch: we don’t have long-term data yet. The ORAL Surveillance trial followed patients for up to four years. Most newer studies are under a year. The FDA has mandated a 10-year safety study for all JAK inhibitors. Until then, assume all of them carry similar risks.Real Patient Experience: The Trade-Off
A 52-year-old woman with severe psoriatic arthritis tried six biologics before switching to upadacitinib. Her skin cleared up in weeks. She went from using a cane to hiking again. But after six months, she got shingles. She recovered, but it scared her. She still takes the drug - but now she gets a shingles booster every year, checks her cholesterol monthly, and avoids long flights without moving her legs. Her story isn’t rare. According to a 2023 Arthritis Foundation survey, 82% of patients who avoided infections and clots said the drug worked better than anything else they’d tried. But 57% still worry about blood clots. And 68% fear infection. That’s not fearmongering - that’s reality.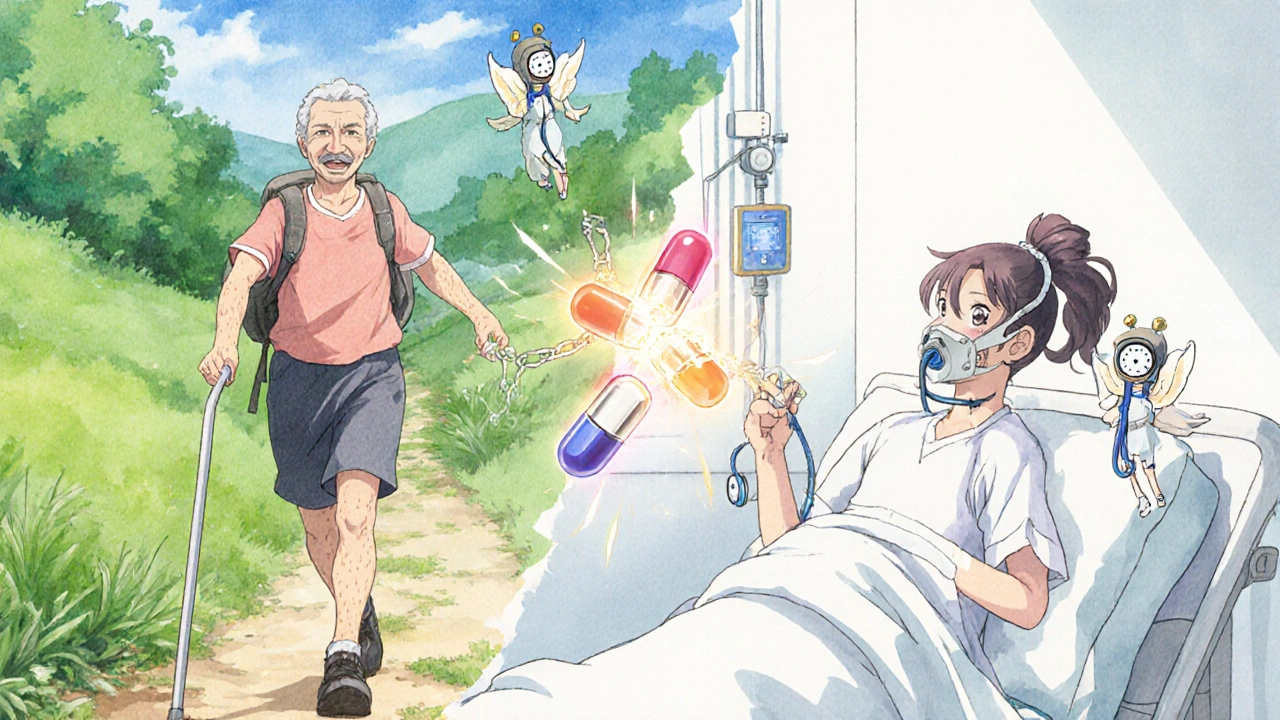
What Comes Next?
The field is moving toward more targeted drugs. TYK2 inhibitors - like deucravacitinib - are already approved for psoriasis and appear to have a cleaner safety profile. They don’t block JAK2 as much, so clot and infection risks may be lower. They’re not yet approved for rheumatoid arthritis or ulcerative colitis, but trials are underway. For now, JAK inhibitors are still a tool - but only for the right patient. They’re not first-line. They’re not for everyone. They’re not a shortcut. They’re a calculated risk.What to Do If You’re on a JAK Inhibitor
- Get your blood tests done on time - no skipping.
- Know the signs of infection: fever, chills, sore throat, cough, painful urination, red/swollen skin.
- Know the signs of a clot: swelling, warmth, or pain in one leg; sudden shortness of breath; chest pain; rapid heartbeat.
- If you’re over 65, smoke, or have a history of clots or heart disease - talk to your doctor about switching.
- Don’t ignore symptoms. If something feels off, call your rheumatologist - don’t wait for your next appointment.
What to Do If You’re Considering One
- Ask: Have I tried at least one TNF inhibitor or biologic first?
- Ask: Do I have any risk factors for clots or infection?
- Ask: Can I commit to monthly blood tests and regular check-ins?
- Ask: Is there a safer alternative - like a different biologic or a TYK2 inhibitor?
There’s no shame in choosing a slower, safer path. The goal isn’t just to reduce joint pain - it’s to live longer, healthier, and without unexpected hospitalizations.
Can JAK inhibitors cause cancer?
Yes. The FDA’s black box warning includes cancer risk. In the ORAL Surveillance trial, patients on tofacitinib had a 54% higher risk of cancer (excluding skin cancer) compared to TNF inhibitors. The most common cancers were lung, lymphoma, and breast cancer. This risk appears higher in older patients and those with a history of smoking or prior cancer. Regular skin checks and cancer screenings are now part of standard care for anyone on these drugs.
Are JAK inhibitors safe for people with diabetes?
Diabetes increases your risk of infection - especially skin and urinary tract infections. JAK inhibitors make that worse. If you have diabetes, your doctor should carefully weigh whether the benefits outweigh the risks. Many rheumatologists avoid prescribing them to patients with poorly controlled diabetes. If you do start one, you’ll need tighter blood sugar monitoring and more frequent infection screenings.
How soon after starting a JAK inhibitor do side effects appear?
Infections can happen anytime, but most serious ones occur within the first 6 months. Blood clots often appear within the first 3 to 6 months - especially after long periods of immobility, like travel or bed rest. Cholesterol levels rise within 4 weeks. That’s why labs are checked at 4 and 12 weeks. Don’t assume you’re safe just because you’ve been on it for a year.
Can I take JAK inhibitors with other immunosuppressants?
No. Combining JAK inhibitors with other immunosuppressants - like methotrexate, azathioprine, or corticosteroids - increases infection risk dramatically. The FDA and EMA warn against this combination. If you’re on methotrexate and your doctor wants to switch you to a JAK inhibitor, they’ll typically stop methotrexate first. Never combine them without explicit approval from your rheumatologist.
What happens if I stop a JAK inhibitor?
Your symptoms may return within weeks. JAK inhibitors don’t cure disease - they suppress it. Stopping suddenly doesn’t cause withdrawal, but flare-ups are common. If you stop because of an infection or clot, your doctor will usually wait until you’re fully recovered before switching to another drug - often a TNF inhibitor or a newer agent like a TYK2 inhibitor. Don’t restart on your own.







Nate Girard October 31, 2025
I started tofacitinib last year and honestly? It’s been a game-changer for my psoriatic arthritis. I can finally play with my kids without wincing. But after six months, I got shingles-thankfully caught early. Now I get the booster yearly, check my cholesterol, and avoid long flights without moving. It’s not perfect, but it’s worth it for me. Just know your risks and stay on top of labs.
Carolyn Kiger November 1, 2025
My mom’s on baricitinib and she’s 71. Her doctor said no because of the ORAL Surveillance data. She was devastated-she’d tried five biologics. But honestly? I’m glad they held the line. Better slow and safe than fast and in the ICU.
krishna raut November 1, 2025
JAK inhibitors increase VTE risk 2.3x. Screen for TB. Avoid live vaccines. Check lipids monthly. That’s it.
Prakash pawar November 3, 2025
Look man we’re all just meat sacks trying to outrun death with pills and science. JAK inhibitors? They’re like hacking into your immune system’s wifi and changing the password. Cool until the hacker turns out to be your own body screaming for help. I mean cmon we’re talking about people getting fungal pneumonia because their body forgot how to fight. Is this really progress or just fancy placebo with a black box warning? 🤔
MOLLY SURNO November 3, 2025
Thank you for this comprehensive overview. The data presented is both alarming and necessary for informed consent. I appreciate the emphasis on monitoring protocols and the clear distinction between risk factors. This level of detail should be standard in every patient consultation.
Erin Corcoran November 4, 2025
OMG I just got my bloodwork back and my platelets dropped 20% 😱 I’ve been on upadacitinib 8 months and didn’t realize how fast things can change. My doc said to hold it until next week’s labs. I’m scared but also so grateful I didn’t ignore the fatigue. #JAKinhibitors #healthalert
shivam mishra November 4, 2025
From India, we see a lot of TB cases. The screening protocol is non-negotiable here. Also, most patients don’t know about the cholesterol spike-it’s common to see LDL jump 30-40% in 6 weeks. Always pair JAK inhibitors with statins if possible. And no, you can’t combine with methotrexate. Seen too many patients crash from infections.
Scott Dill November 5, 2025
My cousin took tofacitinib and got a PE after a road trip. She was 58, healthy, no history. They didn’t even think it was a clot until she collapsed. Now she’s on blood thinners and hates that she ever took it. I told my doc I’m sticking with biologics. No thanks.
Arrieta Larsen November 7, 2025
My rheumatologist refused to prescribe it after I mentioned my dad had lung cancer. I get it. But it’s frustrating when the only thing left that works is the one they won’t let you take.
Mike Gordon November 7, 2025
Just got back from my 12-week blood test. Cholesterol up. Platelets down. WBC normal. Doc says keep going but watch it. I’m 53, non-smoker, no clots. Still, I’m thinking about switching to a TYK2 inhibitor when it’s approved for UC. I’m not dying for relief.
Kathy Pilkinton November 9, 2025
Oh wow. So the drug that makes you walk again also makes you a statistic? Congrats, Big Pharma. You turned a life-saving pill into a Russian roulette game with extra side effects. And now we’re supposed to be grateful you put a black box on it? Please. If I’m going to die, I’d rather die in pain than in a hospital because your ‘innovation’ got me.