Medication Risk Checker for Severe Pancreatitis
Check Your Medication Risks
Identify if any of your current medications could trigger severe pancreatitis. This tool references the 8 high-risk drug classes discussed in the article.
Your Medication Risk Assessment
What Is Drug-Induced Severe Pancreatitis?
Severe pancreatitis from medications is when a drug triggers dangerous inflammation in your pancreas - an organ that helps digest food and control blood sugar. Unlike gallstones or alcohol, which are common causes, this form comes from something you took on purpose: a blood pressure pill, a diabetes med, a cholesterol drug, or even an arthritis treatment. It’s rare - only about 1 in 30 cases of acute pancreatitis - but it’s deadly serious. About 15% to 30% of people who develop this condition die if it’s not caught early. The good news? If you stop the medicine fast enough, your pancreas can heal completely.
How Do You Know It’s Happening?
The biggest red flag is sudden, intense pain in the upper belly that radiates to your back. It doesn’t come and go - it’s constant, often worse after eating, and can wake you up at night. You might also feel nauseous, vomit, or have a fever. But here’s what makes it tricky: these symptoms look exactly like gallstones, stomach bugs, or even heartburn. That’s why so many people are misdiagnosed.
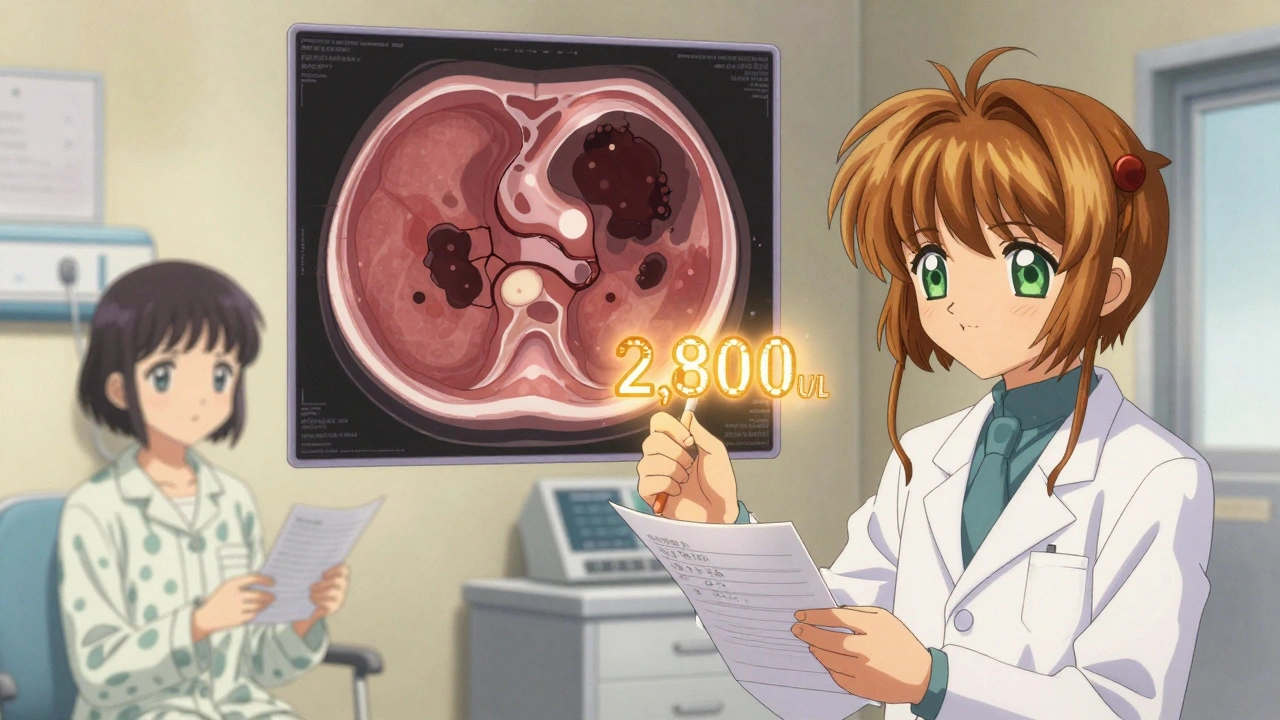
Doctors rely on two key things to confirm it: blood tests and imaging. Your lipase level - a digestive enzyme made by the pancreas - will be at least three times higher than normal. A normal lipase is under 60 U/L. If it’s over 180, that’s a major warning. A CT scan will show swelling, fluid around the pancreas, or even dead tissue (necrosis), especially if more than 30% of the organ is affected. If you’re on any of the high-risk medications and have this pain, ask for a lipase test right away. Don’t wait.
Which Medications Are Most Likely to Cause It?
Not all drugs carry the same risk. Eight classes have strong evidence linking them to severe pancreatitis:
- ACE inhibitors - especially lisinopril and enalapril (used for high blood pressure)
- Diuretics - like furosemide (Lasix) and hydrochlorothiazide
- Diabetes drugs - exenatide (Byetta), sitagliptin (Januvia), and newer SGLT2 inhibitors like dapagliflozin and canagliflozin
- Statins - simvastatin and atorvastatin (cholesterol-lowering pills)
- Immunosuppressants - azathioprine and valproic acid (used for Crohn’s, lupus, epilepsy)
- Oral contraceptives - especially those with ethinyl estradiol
- Antiretrovirals - didanosine (used in HIV treatment)
Valproic acid and azathioprine are the worst offenders. One study found that 22% of people on valproic acid developed necrotizing pancreatitis - meaning parts of the pancreas died. That’s far higher than most other drugs. Even statins, which millions take safely for years, can suddenly trigger it. One Reddit post from a doctor described a 62-year-old man on simvastatin for three years who suddenly had a lipase level of 2,800. He improved within three days after stopping the pill.
Why Is It So Dangerous?
Severe pancreatitis isn’t just pain. It can lead to organ failure. Your kidneys, lungs, or heart may stop working properly. You can develop infections in dead pancreatic tissue. You might need surgery. The mortality rate for drug-induced severe pancreatitis is 28% within 30 days - higher than gallstone-related cases. Why? Because patients are often older, taking multiple meds, and the drugs themselves can make treatment harder. For example, if you’re on blood thinners or immunosuppressants, your body can’t fight infection as well.
Another problem: delayed diagnosis. On PatientsLikeMe, 68% of people with drug-induced pancreatitis said it took weeks before they got the right answer. One woman on azathioprine for Crohn’s was told her pain was “just gastritis.” By the time they scanned her, 40% of her pancreas was dead. She spent three weeks in the ICU.
How Is It Treated?
There’s no magic pill. Treatment is about support - letting your body heal while preventing collapse.
- Stop the drug immediately. This is the single most important step. Delaying by more than 24 hours increases your risk of complications by 37%.
- IV fluids. You’ll get 250-500 mL per hour of saline to keep your blood pressure up and your pancreas perfused. Too little fluid means more tissue death.
- Pain control. Acetaminophen is first-line. If that’s not enough, doctors use morphine - but carefully. Too much can cause spasms in the pancreatic duct.
- Early feeding. You won’t eat for the first day or two. But after 24-48 hours, if you can’t tolerate food by mouth, you’ll get nutrition through a tube placed past your stomach into your small intestine. This reduces infection risk and speeds recovery.
- Antibiotics only if infected. You don’t get them just because you have pancreatitis. Only if a CT scan shows infected dead tissue - then meropenem is the go-to drug.
Most people improve in 7-10 days if caught early. But if you develop necrosis or organ failure, you could be in the hospital for weeks - or longer.

What Happens After You Recover?
If you had drug-induced pancreatitis, you should never take that medication again. Ever. Even if you feel fine, restarting it can cause a second, even deadlier episode. Your doctor will need to find alternatives. For example:
- If lisinopril caused it, switch to an ARB like losartan.
- If sitagliptin triggered it, consider metformin or GLP-1 agonists like semaglutide (which have lower risk).
- If you’re on azathioprine, talk to your doctor about mycophenolate - it has a lower pancreatitis risk.
Some people worry about long-term damage. The good news? Most recover fully. Your pancreas regenerates. But if you had necrosis or multiple episodes, you might develop diabetes or chronic pancreatitis later. That’s why follow-up with a gastroenterologist is critical.
Why Is This Under-Recognized?
Doctors don’t always think of drugs as the cause. Many assume it’s gallstones or alcohol - especially in older patients. But polypharmacy is rising. The average person over 60 takes 5.2 medications. That’s a lot of chances for one to go wrong.
There’s also confusion about causality. One expert says up to 40% of reported cases are probably coincidence - like a statin user getting pancreatitis just by bad luck. But when a patient develops symptoms 7-14 days after starting a new drug, and the lipase spikes, and the pain vanishes after stopping it - that’s not luck. That’s a pattern.
The FDA and EMA are finally catching on. They’ve added black box warnings to diabetes drugs like exenatide and SGLT2 inhibitors. Hospitals are starting to build alerts into electronic records - if you’re on azathioprine and your lipase is high, the system flags it.
What Should You Do?
If you’re on any of the high-risk medications and experience persistent upper abdominal pain - especially if it radiates to your back - don’t wait. Don’t take antacids and hope it goes away. Go to urgent care or the ER. Ask for a lipase test. If it’s high, push for a CT scan. Tell them you’re on medication that could be the cause. Bring a list of everything you’re taking.
If you’ve had pancreatitis before and are prescribed a new drug, ask: “Has this been linked to pancreatitis?” If your doctor says no, ask for the evidence. If they brush you off, get a second opinion.
Drug-induced pancreatitis is preventable. It’s treatable. But only if you speak up - and if your doctor listens.







Saket Modi December 1, 2025
lol why are we even talking about this? just stop taking all meds and eat kale bro 🤡
Chris Wallace December 3, 2025
I've been on atorvastatin for six years and never had an issue, but I know someone who developed pancreatitis after starting sitagliptin. The timing was too perfect - pain started 10 days after the script was filled, lipase hit 2,100, and within 48 hours of stopping it, the pain vanished. It’s not always coincidence. Sometimes the system ignores the signal because the drug’s profit margin is too high to admit it.
Sandi Allen December 5, 2025
This is a classic case of pharmaceutical greed! They know statins and SGLT2 inhibitors cause pancreatitis - the FDA’s own database has over 3,000 reports! But they bury it under "rare" and "correlation ≠ causation" - until someone dies, then they slap on a black box warning and charge you $500 for the "new improved" version! Wake up! The system is rigged! And don’t even get me started on how they push these drugs to seniors on Medicare - it’s elder abuse with a prescription pad!!!
alaa ismail December 6, 2025
I appreciate the breakdown - it’s scary how many people just ignore upper abdominal pain because "it’s probably just gas." I had a friend on lisinopril who waited three weeks because she thought it was acid reflux. By the time she got scanned, her pancreas was 35% necrotic. She’s fine now, but she had to get a feeding tube and spent a month in the hospital. Point is: if it hurts like hell and doesn’t go away, don’t Google it. Go get a lipase test. It takes five minutes.
ruiqing Jane December 6, 2025
I’m a nurse in internal medicine, and I’ve seen this exact scenario play out too many times. Patients come in with classic symptoms - constant epigastric pain radiating to the back, nausea, elevated lipase - and the first thing the resident says is, "Did you drink?" or "Any gallstones?" No one asks about meds. Not until the patient says, "Oh, I started that new diabetes pill last month." Then it clicks. We need mandatory med-reconciliation flags in triage. It’s not complicated. Just ask. It saves lives.
Carolyn Woodard December 7, 2025
The epistemological challenge here lies in the ontological ambiguity of iatrogenic causality. While temporal proximity and biomarker correlation (e.g., lipase > 3x ULN) suggest pharmacological etiology, the absence of a mechanistic pathway - particularly for statins, which lack direct pancreatic toxicity in vitro - introduces a confounding variable: latent susceptibility. Could it be that polypharmacy induces mitochondrial dysfunction in pancreatic acinar cells, rendering them vulnerable to otherwise benign compounds? The literature is sparse on this. We need prospective cohort studies with pharmacogenomic stratification - not anecdotal Reddit case reports. But I concede: when the drug stops and the pain vanishes, Occam’s razor cuts deep.
Zoe Bray December 8, 2025
It is imperative to emphasize that the cessation of the implicated pharmacological agent constitutes the single most critical intervention in the management of drug-induced acute pancreatitis. Delayed discontinuation is associated with a statistically significant increase in the incidence of systemic inflammatory response syndrome (SIRS), multi-organ dysfunction syndrome (MODS), and mortality. Furthermore, the administration of enteral nutrition via nasojejunal tube within 48 hours has been demonstrated in randomized controlled trials to reduce infectious complications and length of hospital stay. Clinicians must be vigilant in reviewing medication histories - particularly in geriatric populations on ≥5 medications - and consider drug-induced pancreatitis in the differential diagnosis even in the absence of traditional risk factors.
Shubham Pandey December 9, 2025
Just stop the drug. That’s it. No magic. No drama.