G6PD Deficiency: What You Need to Know
When working with G6PD deficiency, a hereditary shortage of the enzyme glucose‑6‑phosphate dehydrogenase that protects red blood cells from oxidative damage. Also known as Glucose‑6‑Phosphate Dehydrogenase deficiency, it can cause sudden anemia when certain triggers are introduced. In simple terms, your red cells lose a key shield, so anything that creates extra oxidative stress can break them apart.
The antibiotic Dapsone, a sulfone drug used for leprosy and some skin conditions is a classic trigger because it creates oxidative stress that overwhelms the weak enzyme system. If you have G6PD deficiency, taking Dapsone often leads to the rapid destruction of red blood cells, a process known as hemolysis.
On the safer side, the JAK inhibitor Baricitinib, used for rheumatoid arthritis and COVID‑19 does not usually provoke hemolysis, making it a better option for patients with this deficiency. Doctors often prefer drugs that avoid oxidative pathways, and Baricitinib fits that bill.
Hemolytic anemia, the rapid breakdown of red blood cells leading to fatigue, jaundice, and dark urine is the most common clinical outcome when a trigger is missed. The body’s response is swift: bilirubin spikes, the spleen works overtime, and you feel weak within hours.
Key Topics Covered
Beyond drug safety, G6PD deficiency encompasses a few other important pieces. First, the genetic aspect: the condition follows an X‑linked inheritance pattern, meaning males are usually affected while females can be carriers. Second, everyday triggers: foods like fava beans, infections, and even certain over‑the‑counter pain relievers can cause trouble. Finally, testing: a simple blood test measures enzyme activity and confirms the diagnosis.
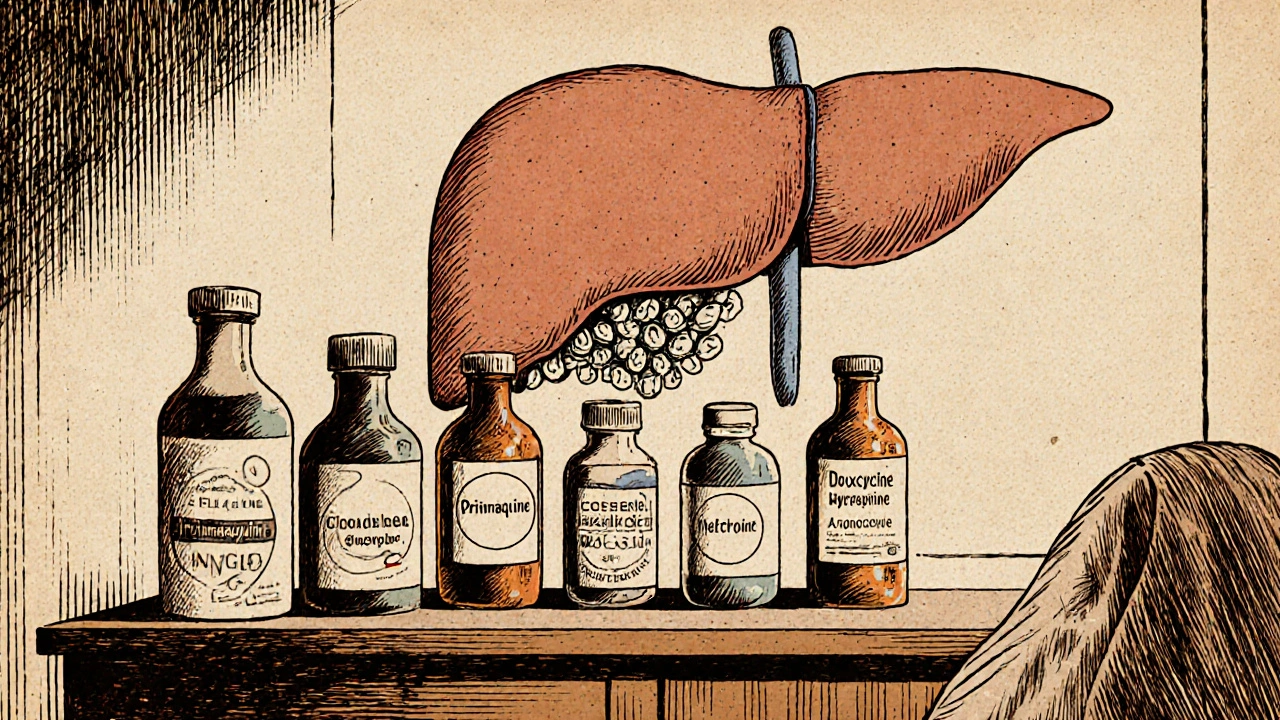
Because the list of risky substances is long, many patients keep a personal “trigger list.” Write down any medication that mentions “sulfa,” “nitrofurantoin,” or “primaquine,” and share it with every pharmacist. Apps and printable cards are handy tools for quick reference.
Management also includes preventive steps. Staying hydrated, avoiding unnecessary stress, and having a clear action plan for an acute hemolytic episode can cut down emergency visits. If you notice dark urine or sudden fatigue after a new drug, seek medical care right away – early treatment with fluids and, if needed, a blood transfusion can keep complications minimal.
The articles below dive deeper into each of these points. You’ll find a detailed comparison of Dapsone versus safer alternatives, an explanation of how Baricitinib works without triggering hemolysis, and practical advice on living day‑to‑day with G6PD deficiency. Use this curated collection to answer your questions, spot the right medication, and stay one step ahead of potential triggers.
Primaquine vs Other Antimalarials: Detailed Comparison and When to Use Each
A thorough side‑by‑side comparison of primaquine with chloroquine, mefloquine, doxycycline, and atovaquone‑proguanil, covering uses, safety, cost, and how to choose the right antimalarial.