Rheumatoid Arthritis – What You Need to Know
When dealing with Rheumatoid Arthritis, a chronic autoimmune condition that primarily attacks the joints. Also known as RA, it causes swelling, stiffness, and long‑term joint damage if left unchecked. Autoimmune disease, a disorder where the immune system mistakenly attacks the body drives this process, making early detection crucial. The disease doesn’t just stay in the joints; lungs, heart, and eyes can feel the impact too. Understanding how DMARDs, Disease‑Modifying Anti‑Rheumatic Drugs that slow disease progression and biologic therapy, targeted medicines that block specific immune pathways work helps you choose the right plan, while NSAIDs, non‑steroidal anti‑inflammatory drugs for pain relief keep daily discomfort manageable. In short, rheumatoid arthritis encompasses joint inflammation, requires early diagnosis, and is influenced by its autoimmune roots; effective treatment hinges on a mix of DMARDs, biologics, and symptom‑relief options.
Key Factors That Shape Your Rheumatoid Arthritis Journey
First up, the immune system’s misfire. Because it’s an autoimmune disease, the body’s own defenses turn against the synovial lining, creating a thick, painful envelope around the joint. This inflammation triggers the classic morning stiffness that can last an hour or more, and over time it erodes cartilage and bone. Genetics play a subtle role, but lifestyle choices—like smoking—can accelerate the damage. Diagnosis usually involves a combination of blood tests (looking for rheumatoid factor or anti‑CCP antibodies) and imaging, such as X‑rays or ultrasound, to catch erosion early. The earlier you catch it, the better the chances of preserving joint function.
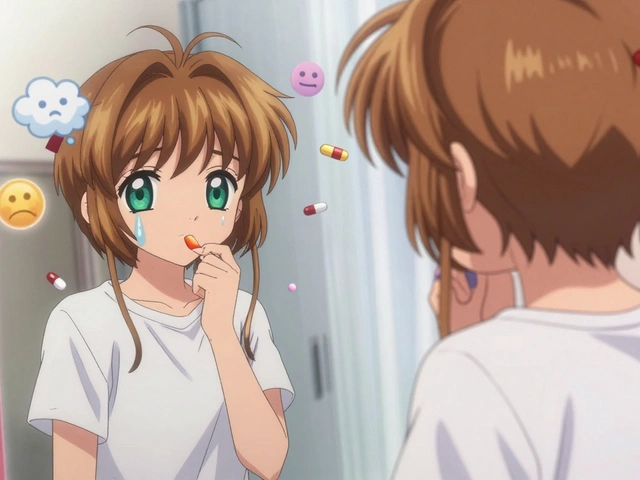
When it comes to treatment, the goal is two‑fold: halt disease progression and keep pain in check. DMARDs such as methotrexate are often the first line because they target the underlying immune activity, not just the symptoms. If the disease stays active despite conventional DMARDs, doctors may move to biologic therapy—agents like TNF inhibitors or IL‑6 blockers—that zero in on specific inflammatory pathways. These biologics have transformed outcomes, allowing many patients to return to work and hobbies they thought were lost. For flare‑ups or milder pain, NSAIDs like ibuprofen or naproxen are a go‑to, offering quick relief while you wait for the longer‑acting drugs to settle in. Physical therapy, regular exercise, and a balanced diet rich in omega‑3 fatty acids also support joint health and reduce systemic inflammation.
All of this information sets the stage for the articles below. You’ll find deeper dives into medication comparisons, lifestyle tweaks, and coping strategies that match the range of topics we cover—from drug safety tips to nutrition advice. Whether you’re newly diagnosed or looking to fine‑tune an existing regimen, the collection ahead gives you practical insights you can start using right away.
Baricitinib Explained: How It Impacts the Immune System
Baricitinib is a JAK inhibitor that modulates the immune system. Learn how it works, approved uses, safety, and how it compares with other drugs in this detailed guide.