Every year, thousands of children end up in emergency rooms because their parents gave them too much medicine - not because they meant to, but because they didn’t realize they were giving the same ingredient twice. It’s not rare. It’s not unusual. It’s active ingredients hiding in plain sight.
Think about it: your child has a fever. You give them Children’s Tylenol. Later, they start coughing, so you grab a bottle of Children’s NyQuil. You’re doing what you think is right - helping them feel better. But both products contain acetaminophen. You just doubled the dose. And that’s not just a mistake. It’s a medical emergency.
Why Double Dosing Is So Dangerous for Kids
Children aren’t small adults. Their bodies process medicine differently. A dose that’s safe for a 60-pound kid could be toxic for a 20-pound toddler. The margin between a helpful dose and a dangerous one is razor-thin - especially with common over-the-counter drugs like acetaminophen and ibuprofen.
Acetaminophen is the most common culprit. It’s in more than 600 different products - cold medicines, fever reducers, allergy pills, even some sleep aids. The liver can only handle so much. Too much acetaminophen, and it starts to break down into a poison. In children under 6, acetaminophen overdose causes nearly half of all acute liver failure cases. And it doesn’t take much. A single extra teaspoon, given twice in a day, can push a child past the safety line.
Other ingredients are just as risky. Diphenhydramine - the sleepy-time drug in Benadryl - shows up in cough syrups, cold remedies, and even some nighttime allergy drops. Double that, and your child could be so drowsy they can’t wake up. Ibuprofen, when doubled, can cause stomach bleeding or kidney damage. Even ADHD meds like Adderall or Ritalin become dangerous if given twice by accident. One parent in Pittsburgh told me their 7-year-old ended up in the ER after getting both a morning ADHD pill and an afternoon cold medicine that contained the same stimulant. That’s not a myth. That’s a real story.
What’s Really in Your Medicine Cabinet?
Here’s the hard truth: you can’t trust the brand name. You can’t trust the flavor. You can’t even trust the bottle shape.
Panadol. Tylenol. FeverAll. Tempra. Excedrin. All of these contain acetaminophen. But they don’t say “acetaminophen” on the front. They say “pain and fever relief.” Or “cold and flu.” Or “sore throat and fever.” And if you’re tired, stressed, or in a hurry - you won’t notice.
Worse, the same ingredient goes by different names. Acetaminophen is also called APAP, paracetamol, or N-acetyl-p-aminophenol. If you don’t know what those mean, you’re not alone. A 2023 study found that 68% of parents didn’t realize those were all the same thing.
And then there’s the liquid problem. A teaspoon isn’t a teaspoon. Household spoons vary by up to 200%. One parent used a regular kitchen spoon, thinking it was a teaspoon, and gave their child three times the intended dose. That’s not negligence. That’s a system failure.
The Simple Fix: Check the Active Ingredient Every Time
You don’t need a pharmacy degree. You don’t need an app. You just need to look at the label - every single time.
Here’s how to do it right:
- Find the “Active Ingredients” section. It’s usually on the back or side of the bottle, in bold. Don’t skip this step.
- Write it down. Use a notebook, your phone, or a sticky note. Write the name of the ingredient and the amount per dose (e.g., “acetaminophen 160 mg per 5 mL”).
- Compare before giving. Before you give any new medicine, check your list. If the active ingredient is already there, don’t give it again.
- Wait at least 4-6 hours between doses. Even if you’re sure you didn’t double up, give your child’s body time to process the medicine.
It sounds simple. But simple doesn’t mean easy. Especially when you’re juggling three kids, a sick partner, and a work deadline. That’s why you need systems.
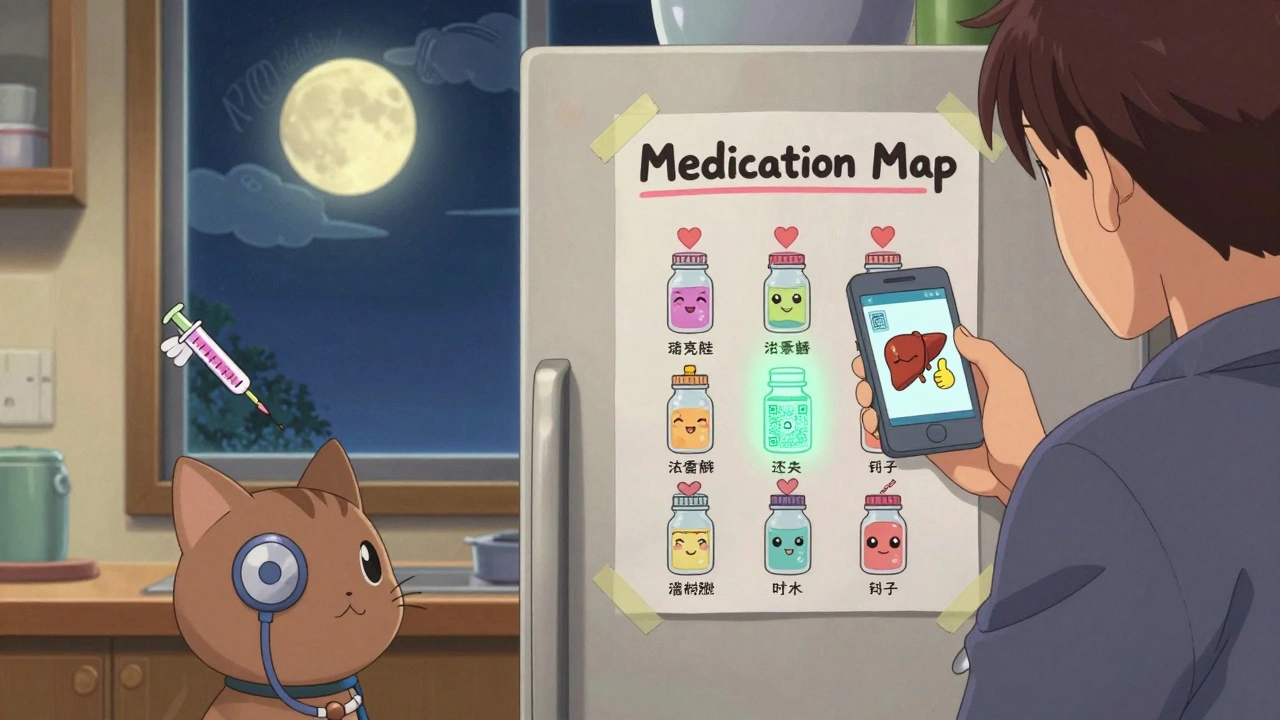
Build a Medication Map
One dad in Ohio created a “medication map” - a one-page chart with all the medicines his kids take. He listed:
- Brand name
- Active ingredient
- Strength (mg per mL)
- Max daily dose
- Time of last dose
He kept it on the fridge. Every time he gave a medicine, he checked the box. Within six months, his family had zero dosing errors. Zero. He didn’t buy fancy gadgets. He just made a habit.
You can do the same. Use a free app like Medisafe or Round Health - they send reminders and flag duplicates. Or just use a paper list. The goal isn’t tech. The goal is awareness.

What to Do If You Accidentally Double Dose
If you realize you gave two doses of the same medicine - don’t panic. But don’t wait either.
Call Poison Control immediately: 1-800-222-1222. It’s free. It’s 24/7. It’s staffed by nurses and pharmacists who’ve seen this exact situation a thousand times. They’ll tell you if it’s an emergency, if you need to go to the ER, or if you just need to watch for symptoms.
Symptoms to watch for:
- Acetaminophen overdose: nausea, vomiting, pale skin, loss of appetite, right-side abdominal pain
- Diphenhydramine overdose: extreme drowsiness, trouble waking up, fast heartbeat, flushed skin, hallucinations
- Ibuprofen overdose: stomach pain, vomiting, dizziness, ringing in the ears
Don’t wait for symptoms. If you’re unsure, call. Better safe than sorry.
What the Experts Say
Dr. Robert Hiriart, a pediatric pharmacologist, says: “The prescribed dose is often calculated down to the gram based on your child’s weight. Even a little extra can double the risk of side effects.”
The American Academy of Pediatrics now says: “Always check the active ingredient before giving any new medicine.” That’s not a suggestion. That’s their official guideline.
And here’s the kicker: parents who use this simple check reduce double dosing by 71%. That’s not a guess. That’s from a 2023 study in Pediatrics.
What to Avoid
Some habits make double dosing worse:
- Alternating Tylenol and Advil for fever - this increases the chance of mixing up doses by 47%. Stick to one unless your doctor says otherwise.
- Using kitchen spoons - they’re not accurate. Always use the dosing cup or syringe that came with the medicine.
- Assuming “natural” or “herbal” means safe - some herbal cough syrups contain hidden acetaminophen or stimulants.
- Buying multiple brands for different symptoms - if you need a cold medicine, get one that covers everything. Don’t stack three separate bottles.
What’s Changing - and What You Should Know
Good news: things are getting better. Starting in December 2025, the FDA will require all children’s OTC medicines to list active ingredients in a standard format - bold, clear, and consistent. No more hiding it in tiny print.
Some brands are already doing it. Johnson & Johnson and Procter & Gamble now put QR codes on their bottles. Scan it, and you’ll see a breakdown of all active ingredients - in plain language.
Amazon Pharmacy’s new “MedCheck” feature scans your order and warns you if you’re buying two products with the same ingredient. It’s already stopped 12,000 potential overdoses in six months.
But technology won’t fix this alone. You still have to look. You still have to check. Because no app can replace your eyes - and your attention.
Final Thought: It’s Not About Being Perfect
You’re not going to remember every ingredient all the time. You’re going to get tired. You’re going to miss a step. That’s okay.
What matters is that you build the habit. Keep a list. Check the label. Call Poison Control if you’re unsure. You don’t need to be a pharmacist. You just need to be careful.
Because when it comes to your child’s medicine - the difference between safe and dangerous isn’t always obvious. But it’s always there. And you’re the only one who can catch it.
How do I know if two medicines have the same active ingredient?
Look at the “Active Ingredients” section on the Drug Facts label. Even if the brand names are different - like Tylenol and Children’s NyQuil - if both list “acetaminophen” or “APAP,” they’re the same. Write down the ingredient and the dose per milliliter. Compare before giving any new medicine.
Can I give my child both Tylenol and Advil for fever?
The American Academy of Pediatrics advises against alternating acetaminophen and ibuprofen in children under 3 years unless directed by a doctor. Doing so increases the chance of accidental double dosing by 47%. Stick to one medication unless your pediatrician gives specific instructions.
What should I do if I think I gave my child too much medicine?
Call Poison Control immediately at 1-800-222-1222. They’re available 24/7 and can tell you whether you need to go to the ER. Don’t wait for symptoms. Don’t try to induce vomiting. Don’t give milk or charcoal unless they say so. Just call.
Are liquid medicines measured the same way?
No. Always use the dosing tool that came with the medicine - a syringe or cup marked in milliliters (mL). Household teaspoons vary from 2.5 mL to 7.5 mL, which can lead to triple dosing. Never use a regular spoon.
Why do some medicines have different names for the same ingredient?
Acetaminophen is sold under many names: APAP, paracetamol, N-acetyl-p-aminophenol. This confuses parents. The FDA is changing this - by 2025, all labels must use “acetaminophen” as the primary term. Until then, learn these names and check every label.
Do all cold medicines contain acetaminophen?
About 89% of multi-symptom cold and flu medicines for children contain acetaminophen. That includes popular brands like Children’s NyQuil, Theraflu, and Vicks products. Never assume a cold medicine is “just for cough” - always check the active ingredients.
Is it safe to use expired children’s medicine?
No. Expired medicine may not work as intended, and the concentration can change over time. For children, this increases the risk of under- or overdosing. Always check expiration dates and dispose of old medicines properly.
Can I give my child adult medicine if I cut the dose in half?
Never. Adult medicines are formulated differently and often contain ingredients not safe for children. Even if you reduce the dose, the concentration of other ingredients - like alcohol or artificial sweeteners - can still be harmful. Always use medicine made for children.
Next Steps: What to Do Today
Here’s your quick action plan:
- Go to your medicine cabinet right now.
- Find every children’s medicine - even the ones you haven’t used in months.
- Write down the active ingredient and strength for each one.
- Put that list on your fridge or phone.
- Next time you give medicine, check it before you give it.
You don’t need to be perfect. You just need to be aware. And that one habit - checking the active ingredient - could save your child’s life.








sharon soila December 12, 2025
Every parent should read this. I didn’t know acetaminophen was in so many things. I just thought Tylenol and NyQuil were different. I’m printing this out and taping it to the fridge. My kids are 3 and 5. I can’t afford to make a mistake.
Thank you for writing this. You saved me from a disaster I didn’t even know was coming.
nina nakamura December 13, 2025
You’re lucky you didn’t kill your kid already. People are idiots. Just read the label. It’s not hard. Stop making excuses for being lazy.
Sheldon Bird December 14, 2025
This is such an important post. I used to alternate Tylenol and Advil like it was a game. Then my niece had a scare last year. Now I have a little chart on my phone. I even set a reminder before every dose.
It’s not about being perfect. It’s about being present. And that’s something we can all do.
Willie Onst December 14, 2025
Man I remember when I gave my son two different cold meds and he slept for 14 hours straight. We thought he was just really tired. Turned out it was diphenhydramine overload. Scared the crap out of us.
Now I keep a list. I don’t even trust myself anymore. And I’m not even a parent. I just help out with my nephew. If it works for me, it’ll work for you.
Also - QR codes on bottles? That’s genius. I hope all brands do that soon.
Jennifer Taylor December 14, 2025
THEY’RE HIDING IT ON PURPOSE. I SWEAR TO GOD THE PHARMA COMPANIES WANT THIS TO HAPPEN. WHY ELSE WOULD THEY USE 12 DIFFERENT NAMES FOR ACETAMINOPHEN? WHY ISN’T THERE A FEDERAL LAW TO FORCE ONE NAME? WHY ARE WE STILL USING TEASPOONS? THIS IS A CONSPIRACY. THEY WANT US TO MESS UP SO THEY CAN SELL MORE MEDS.
AND DON’T TELL ME TO CALL POISON CONTROL - THEY’RE IN THE POCKET OF BIG PHARMA TOO. I SAW A VIDEO ON TIKTOK ABOUT A NURSE WHO WAS FIRED FOR TELLING THE TRUTH.
MY KID IS ON A DIY HERBAL REGIMEN NOW. NO MORE CHEMICALS. JUST HONEY AND GINGER.
JUST SAYIN’.
Shelby Ume December 15, 2025
Thank you for writing this with such clarity. I’m a nurse, and I see this every week in the ER. Parents aren’t careless - they’re overwhelmed. And the labeling? It’s a mess.
I give every new parent I work with a laminated card with the top 5 active ingredients and what they do. No apps. No tech. Just a card. Simple. Effective.
Also - never use a kitchen spoon. Ever. I’ve seen kids hospitalized because someone thought ‘a teaspoon’ meant what they used for coffee.
Jade Hovet December 17, 2025
OMG I JUST REALIZED I DID THIS LAST WEEK 😭😭😭 I GAVE MY DAUGHTER TYLENOL FOR FEVER THEN GAVE HER COUGH SYRUP BECAUSE SHE WAS COUGHING AND IT HAD ACETAMINOPHEN TOO 😭 I DIDN’T EVEN THINK TO CHECK 😭
THANK YOU FOR THIS POST I’M GOING TO MAKE A LIST RIGHT NOW AND PUT IT ON MY PHONE AND MY FRIDGE AND MY TOILET LID 😂
PS I’M GOING TO BUY THOSE DOSING SYRINGES TOO I’M SO SORRY TO EVERYONE I’VE BEEN A BAD PARENT 😭❤️
nithin Kuntumadugu December 19, 2025
USA so dumb. In India we just use one medicine. No need for 600 brands. All same stuff. You people overcomplicate everything. Also why you need QR code? Just read. Simple. You lazy. Pharma companies make you dumb.
John Fred December 19, 2025
As a pediatric pharmacist, I can’t stress this enough: APAP = acetaminophen = paracetamol. If you don’t know this, you’re one mistake away from liver failure.
Also - the 4-6 hour window? Non-negotiable. Even if your kid is still feverish. The liver needs time. You’re not helping by giving more. You’re just poisoning them slowly.
And yes - the FDA’s 2025 changes are long overdue. But until then? Your eyes are your best tool.
Harriet Wollaston December 20, 2025
I’m a single mom of three. I work two jobs. I don’t have time to memorize drug names. But I do have time to write one line on a sticky note.
I keep it on my bathroom mirror. ‘Check the ingredient. Always.’
It’s not about being perfect. It’s about being present. And I’m trying.
Thank you for reminding me I’m not alone in this.
Lauren Scrima December 22, 2025
Wow. So you’re saying… we’re supposed to *read*? Like, actually read the tiny print? On a bottle? In the middle of the night? When our kid is screaming? Oh my god. What a shocker. I’m sure the FDA didn’t think of this. 🙄
Tommy Watson December 23, 2025
This whole thing is overblown. My cousin’s kid took two meds and was fine. You people panic over everything. Just let kids be kids. They’re tougher than you think. Stop treating them like glass.
Donna Hammond December 24, 2025
I’m a pediatric nurse and I’ve seen 12 cases of acetaminophen toxicity in kids under 5 this year alone. Every single one was preventable.
The real tragedy isn’t the overdose - it’s that it’s so avoidable. You don’t need to be a genius. You just need to pause. Look. Write it down.
And if you’re tired? That’s when you need the list the most.
Please don’t wait until it’s too late.
Richard Ayres December 25, 2025
This is one of the most thoughtful and practical guides I’ve read on pediatric medication safety. It’s not about fear. It’s about responsibility. And responsibility doesn’t require perfection - just consistency.
I’ve started keeping a digital log in Notion for my nieces’ meds. It syncs across devices. Even my sister, who hates tech, uses it now. Simple systems win.
Thank you for making this accessible. This is public health done right.
Karen Mccullouch December 26, 2025
I can’t believe people are still falling for this. The government and Big Pharma are pushing this fear so they can sell you more expensive ‘safe’ meds. I gave my kid generic stuff for years. No problems. You’re being manipulated. Wake up.