Switching from a brand-name drug to its generic version should be simple: same active ingredient, same dose, same effect. But for millions of Americans, it’s anything but. A 2023 CDC report found that medication adherence drops by an average of 15% after a brand-to-generic switch - not because the medicine doesn’t work, but because patients believe it doesn’t. This isn’t just about cost. It’s about trust, perception, and how we’re told to think about the pills we take every day.
Why People Stop Taking Their Generic Medication
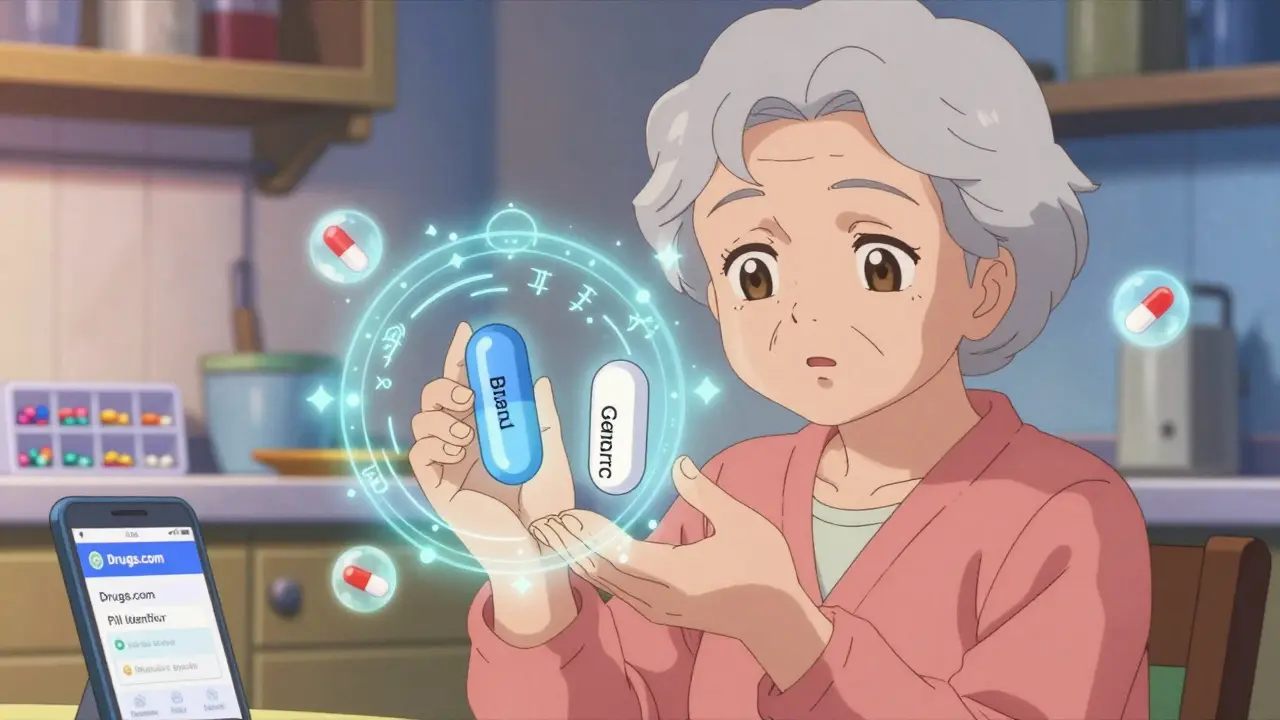
Let’s say you’ve been taking a blue capsule for high blood pressure for years. Then one day, your pharmacy gives you a white oval pill instead. Same prescription. Same doctor. Same insurance. But you notice the shape, the color, even the tiny imprint on the pill is different. Suddenly, you start wondering: Is this really the same?
You’re not alone. A 2020 University of Michigan study found that 28.4% of older adults became confused or anxious after a pill change - even when the active ingredient was identical. That confusion leads to skipped doses, reduced confidence, and sometimes, complete discontinuation. In one 2018 study, patients given identical placebo pills labeled as “generic” reported 18.3% more pain and were 31.6% more likely to take extra pills from their medicine cabinet - not because the placebo was stronger, but because they believed it was weaker.
This isn’t just psychology. It’s biology. The body responds to expectations. A 2014 double-blind study showed that when people were told they were taking a “generic” version of a painkiller, even if it was the exact same pill, they reported 22% more side effects than when told it was the brand name. The drug didn’t change. Their brain did.
What the FDA Really Says - And What Patients Don’t Know
The FDA requires generics to prove they’re bioequivalent to the brand. That means the amount of drug absorbed into your bloodstream (measured by AUC and Cmax) must fall between 80% and 125% of the brand’s. Sounds loose? It’s not. That same 20% variability exists between batches of the brand-name drug itself. In fact, the FDA says the differences between generic and brand are no greater than the differences between two bottles of the same brand bought six months apart.
But here’s what most patients don’t hear: inactive ingredients can matter. A 2021 JAMA Dermatology study found that 3.7% of patients had allergic reactions or stomach upset due to dyes, fillers, or coatings in generics - not the active drug. That’s why some patients report “new side effects” after switching. It’s not the main ingredient. It’s the extras.
And then there are the drugs where even small changes can be risky. Levothyroxine (for thyroid), warfarin (for blood clots), and certain seizure meds like lamotrigine have a “narrow therapeutic index.” That means the difference between a dose that works and one that doesn’t is tiny. A 2017 NEJM study found a 0.8% higher hospitalization rate in patients switched from brand to generic versions of these drugs. It’s rare, but real. And it’s why some doctors still prefer to keep patients on brand for these conditions.
When Generics Actually Improve Adherence
Here’s the flip side: for many people, switching to generics improves adherence. Why? Cost. A 2018 JAMA Internal Medicine study showed that when patients switched from brand-name statins to generics, adherence went up by 14.2% - because the copay dropped from $120 to $10. For Medicare beneficiaries stuck in the “donut hole,” that difference is life-changing.
And it’s not just statins. A 2015 study of over 300,000 people found that for cholesterol-lowering drugs, generic use led to 62% adherence vs. 53% for brand. For hypertension? The opposite: 47% adherence with generics vs. 59% with brand. Why? Because high blood pressure meds often have more side effects, and patients are more likely to blame the generic for feeling worse - even when the drug is the same.
The lesson? Adherence isn’t about the pill. It’s about the person. For someone struggling to pay for medicine, generics are a lifeline. For someone with a complex condition or deep distrust of generics, the switch can be a trap.
The Role of the Pharmacist - And Why Most Fail
When your prescription is filled, the pharmacist is the last line of defense. But here’s the problem: most don’t have time to explain.
A 2022 audit found that only 28% of pharmacists explained bioequivalence to patients during a brand-to-generic switch. Only 34% talked about why the pill looked different. Just 19% asked, “Do you have any concerns about this change?”
That’s not negligence. It’s system failure. Pharmacists are expected to fill 80+ prescriptions an hour. Counseling takes time - time most don’t have.
But when they do? Results are dramatic. A 2022 meta-analysis found that patients who received a follow-up call from their pharmacist within 72 hours of switching had 31% higher adherence. A simple conversation - “This is the same medicine, just cheaper. The color changed because the manufacturer switched dyes. If you feel anything different, call us” - makes all the difference.
What Works: Proven Best Practices
There are real, evidence-backed ways to improve adherence during transitions. Here’s what works:
- Use pill organizers. A 2023 Kaiser Permanente study found that 47% of patients who used a weekly pill box reported better adherence after switching. Visual cues help overcome confusion from pill appearance.
- Request same-manufacturer generics. If your brand-name drug was made by Pfizer, ask if the generic is made by Pfizer too. Many manufacturers make both. Consistent appearance reduces anxiety.
- Ask for a 30-day supply first. Don’t switch to a 90-day supply right away. Try the generic for a month. If you feel fine, continue. If you notice changes, go back to brand or ask for another generic.
- Use e-prescribing alerts. Systems like Surescripts now flag brand-to-generic switches for pharmacists. When this happens, 22.4% more patients get counseling. Ask your pharmacy if they use this tool.
- Get medication synchronization. If you take multiple drugs, ask your pharmacist to align all refill dates. A 2022 study showed this improved generic adherence by 18.3% - because fewer missed refills mean fewer chances to quit.
What You Can Do Right Now
You don’t need a PhD to protect your adherence. Here’s your quick action plan:
- If you’re switching to a generic, ask your pharmacist: “Is this the same as my old pill? Why does it look different?”
- Check the pill’s imprint with a free tool like Drugs.com Pill Identifier (or ask your pharmacist). Seeing the imprint matches the brand can ease fears.
- Keep a simple log: “Day 1: Took pill. Felt fine.” “Day 3: Slight headache - maybe stress?” Don’t assume every symptom is the drug’s fault.
- Don’t stop without talking to your doctor. If you feel worse, it might be coincidence - or it might be a real reaction. Either way, don’t guess.
- For chronic conditions (thyroid, seizures, heart failure), ask your doctor: “Is this a drug where switching could matter?” If yes, stick with the same generic manufacturer.
The Future: What’s Changing
Starting January 1, 2025, the FDA will require all generic manufacturers to include patient education materials with each prescription - explaining why the pill looks different and how it’s still safe. That’s new. That’s progress.
Also in 2024, the Generic Pharmaceutical Association launched a “Seamless Switch” certification. Drugs with this label will keep the same shape, color, and imprint during brand-to-generic transitions - especially for high-risk meds like thyroid and seizure drugs. This directly tackles the 28.4% confusion rate in older adults.
And AI is stepping in. A 2023 JMIR study tested an app that uses your phone’s camera to verify you took your pill. Patients using it during generic switches had 37% better adherence. The app didn’t change the drug. It changed the trust.
Final Thought: It’s Not About the Pill - It’s About the Story
Generics aren’t inferior. They’re regulated, tested, and approved. But we’ve told ourselves a story: brand = better. That story is outdated. The real question isn’t whether generics work. It’s whether we’re giving patients the facts to believe they do.
Adherence doesn’t fail because of chemistry. It fails because of silence.
Are generic drugs really as effective as brand-name drugs?
Yes, for the vast majority of medications, generic drugs are just as effective. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also prove bioequivalence - meaning they deliver the same amount of drug into your bloodstream within a narrow range (80-125% of the brand). This is the same standard used to test different batches of the brand-name drug itself. Differences in inactive ingredients (like dyes or fillers) can cause rare side effects, but they don’t make the drug less effective.
Why do some people feel worse after switching to a generic?
Most often, it’s not the drug itself - it’s the mind. A well-documented phenomenon called the nocebo effect means people experience side effects because they expect them. If you believe a generic is weaker, your brain may amplify normal sensations - like a slight headache or fatigue - as signs of failure. In rare cases, differences in inactive ingredients (like gluten or dyes) can trigger allergic reactions. If symptoms persist, talk to your doctor. Don’t assume it’s the generic without checking.
Which medications should I avoid switching from brand to generic?
For most drugs, switching is safe. But for medications with a narrow therapeutic index - where small changes in blood levels can cause big effects - caution is advised. These include levothyroxine (thyroid), warfarin (blood thinner), phenytoin and lamotrigine (seizure meds), and cyclosporine (organ transplant). If you’re on one of these, talk to your doctor before switching. Some patients benefit from staying on the same manufacturer’s version, even if it’s generic, to keep pill appearance consistent.
Can I ask for the same generic manufacturer as my brand-name drug?
Yes. Many brand-name manufacturers also make their own generic versions. For example, Pfizer makes both the brand-name Lipitor and its generic, atorvastatin. If you’re switching and want to minimize changes, ask your pharmacist: “Is this made by the same company as my old pill?” You can also check the pill imprint online. Consistent appearance reduces confusion and improves adherence.
How can I tell if my pharmacy switched my generic without telling me?
Check the pill’s shape, color, and imprint - these are listed on the prescription label. If they change unexpectedly, your pharmacy may have switched manufacturers. You can use tools like Drugs.com’s Pill Identifier to compare. If you’re unsure, call your pharmacy and ask: “Was there a change in my medication?” You have the right to know. Some states require pharmacies to notify you before switching, but not all do. Stay informed.
Will my insurance force me to switch to a generic?
Yes - unless your doctor writes a “Do Not Substitute” note. Most insurance plans require you to try the generic first because it’s cheaper. If the generic doesn’t work for you, your doctor can request a prior authorization for the brand. But if you’re worried about switching, talk to your doctor before the change happens. You can also ask your pharmacy to hold off until you’ve had a chance to discuss it.







Brandon Osborne February 9, 2026
This is why America is falling apart. People think a pill changing color means it's a scam. I've been on generics for 12 years-no issues. But no, we gotta coddle every hypochondriac who thinks their blood pressure med is secretly plotting against them. Wake up. The FDA doesn't lie. If you're feeling weird, it's probably your anxiety, not the pill. Stop blaming the system and take your damn medicine.
Lyle Whyatt February 10, 2026
Look, I get it. The psychology here is fascinating. The nocebo effect isn't just some buzzword-it's a full-blown physiological response. I once had a patient swear up and down that her generic metformin made her nauseous, but when we swapped it for the *exact same pill* but labeled as brand-name? No nausea. Zero. The body doesn't know the difference. The mind does. And that's the real battleground. We need to reframe the narrative. It's not about efficacy-it's about perception. We've spent decades marketing brand drugs as premium, so of course people assume generics are inferior. It's branding, not chemistry. The solution? Education. Consistent pill appearance. Pharmacist follow-ups. Not just handing out pills like candy and hoping for the best. We're treating a psychological issue like a pharmaceutical one. That's why adherence tanks. The fix isn't more science. It's more storytelling.
Ken Cooper February 10, 2026
soooo… i just switched to generic lisinopril last month and honestly? felt weird at first. like, my head was foggy? but i kept taking it. turned out i was just stressed from work. then i used drugs.com to check the imprint-same as my old pill, just lighter color. weird how much that helped. also, my pharmacist called me 2 days later. just asked if i was feeling okay. that tiny thing made me feel seen. not just a number. also, i use a pillbox now. game changer. also also, my cat hates when i open the med drawer. she thinks i'm feeding her. lol.
MANI V February 11, 2026
People don't want to admit it, but this is exactly why America is dying. You give someone a cheap pill and they immediately think it's poison. They'd rather pay $120 for a placebo they believe in than take a $10 pill that actually works. This isn't science-it's religion. And we're all just worshiping at the altar of Big Pharma's marketing machine. The FDA? A joke. The system is rigged. You think generics are safe? Then why do they change the shape? Why the colors? Because they want you to doubt. They want you to panic. And when you panic, you go back to the brand. And they make more money. Wake up. This isn't medicine. It's control.
Sam Dickison February 13, 2026
From a clinical pharmacy standpoint, the bioequivalence parameters (80–125% AUC/Cmax) are robust. But what’s often overlooked is inter-individual variability in absorption kinetics. For patients on narrow-therapeutic-index drugs, even minor fluctuations in Cmax can trigger subtherapeutic or toxic outcomes. The key isn't just switching-it's monitoring. TDM (therapeutic drug monitoring) for warfarin or levothyroxine post-switch isn't optional-it’s standard of care. And yes, same-manufacturer generics reduce variability because excipient profiles are consistent. But most prescribers don’t know this. Pharma reps sure do. We need better EHR alerts and mandatory pharmacist counseling protocols. Not optional. Required.
Joseph Charles Colin February 13, 2026
Let’s be real-this isn’t about generics being inferior. It’s about systemic neglect. We’ve turned healthcare into a transactional assembly line. Pharmacists are expected to process 80+ scripts/hour while simultaneously being the emotional anchor for patients terrified of a pill that looks different. That’s not sustainable. And it’s not ethical. The solution isn’t more studies-it’s more staffing. Hire more pharmacists. Fund counseling time. Pay them to talk. A 72-hour follow-up call costs less than one ER visit from a patient who stopped their med. The math is obvious. The will? Not so much. We’re optimizing for profit, not outcomes. And that’s why people die quietly from uncontrolled hypertension because they didn’t trust their own pill.
John Sonnenberg February 14, 2026
I switched to generic atorvastatin last year. First week: headaches. Second week: fatigue. Third week: I was convinced I was having a heart attack. I called my doctor. They said, "It’s probably the pill." I said, "It’s the pill." They said, "It’s the pill." I said, "It’s the pill." I stopped taking it. Then I found out my old brand was made by Pfizer. So I asked for the Pfizer generic. Same pill. Same dose. Same everything. But now? I feel fine. It wasn’t the drug. It was the story. And the story was: "This is cheap. This is trash." Turns out, my brain was the problem. Not the pill. But no one told me that. Until I figured it out myself. This system is broken. And it’s not just about medicine. It’s about trust. And we’ve lost it.
Joshua Smith February 15, 2026
Just wanted to say thanks for this. My mom just switched to generic levothyroxine and she was freaking out. I showed her the FDA guidelines and the pill identifier tool. She checked the imprint-same as before. Then I made her a little chart: "Day 1: Fine" "Day 3: A little tired-maybe winter?" "Day 7: Better than before." She’s been on it for 3 weeks now. No issues. She says she feels more in control. It’s wild how much a little info and a checklist can help. Also, we got her on med sync. Now all her pills come on the same day. She says it feels less like a chore. Small things matter.
Jessica Klaar February 16, 2026
I’m a nurse in rural Texas, and I’ve seen this over and over. An older lady comes in, terrified because her blood pressure pill changed from blue to white. She says, "I don’t trust this one." I sit with her. I show her the label. I call the pharmacy. I get her the same manufacturer’s version. She cries. Not because she’s sick. Because no one ever sat down and explained. We treat meds like a vending machine. But people aren’t machines. They need to feel heard. Not just dosed. I wish every pharmacist had 10 minutes with every patient. It wouldn’t fix the system. But it would save lives.
PAUL MCQUEEN February 17, 2026
So… we’re making a whole article about people being scared of pills? That’s it? That’s the big reveal? People are dumb. They think generic means fake. Newsflash: everything in America is a marketing scheme. The pill doesn’t care. The FDA doesn’t care. The pharmacy doesn’t care. Only the patient cares. And they’re too busy scrolling TikTok to read a 5000-word essay. This whole thing is a solution looking for a problem. Just let people die. The market will sort it out.
glenn mendoza February 18, 2026
Thank you for this thoughtful, evidence-based piece. It’s rare to see a discussion on medication adherence that doesn’t devolve into partisan outrage or pseudoscience. The data is clear: adherence is a behavioral issue, not a pharmacological one. The fact that a simple pharmacist follow-up increases adherence by 31% should be a wake-up call for healthcare systems everywhere. We must prioritize human connection over cost efficiency. Because when a patient stops taking their medication because they’re afraid, it’s not a failure of science-it’s a failure of compassion.
Kathryn Lenn February 20, 2026
Of course the FDA says generics are fine. They’re owned by the same pharma conglomerates that make the brand-name drugs. The whole system is a pyramid scheme. They make you switch to save money, then charge you extra for "special" generics that look like the brand. And don’t get me started on the "Seamless Switch" certification. That’s just branding with a new logo. AI pill-checking apps? That’s not innovation-it’s surveillance. They want to track you. They want to know when you take your pill. So they can sell your data. Or worse-adjust your dose remotely. Wake up. This isn’t healthcare. It’s control.