Malaria Treatment: Effective Strategies and Latest Options
When talking about malaria treatment, the medical approach used to eliminate the Plasmodium parasite that causes malaria. Also known as antimalarial therapy, it combines medication, accurate diagnosis, and prevention measures to clear infection and stop relapse. Antimalarial drugs, chemical agents that kill or inhibit malaria parasites are the core of any cure, while drug resistance, the ability of parasites to survive standard medications constantly reshapes the treatment landscape. Reliable diagnostic testing, methods like rapid diagnostic tests or microscopy that confirm malaria infection is the first step, because you can’t treat what you haven’t proven.
Modern malaria treatment includes several distinct layers. First, a confirmed diagnosis leads to a drug regimen tailored to the species and local resistance patterns. For uncomplicated Plasmodium falciparum infections, artemisinin-based combination therapies (ACTs) dominate because they pair fast‑acting artemisinin with a partner drug that blocks any surviving parasites. In areas where ACT resistance is emerging, alternatives like quinine plus clindamycin or newer drugs such as fosmidomycin may be recommended. Severe cases need intravenous artesunate or quinine, followed by a full oral course. The choice of drug thus reflects the interplay between parasite biology, resistance data, and patient factors.
Key Components of Modern Malaria Care
One semantic truth is that malaria treatment encompasses drug therapy. Without the right medication, even the best prevention fails. Another is that malaria treatment requires accurate diagnosis; mistaking a fever for malaria can lead to overuse of drugs and fuel resistance. Finally, drug resistance influences malaria treatment decisions by forcing clinicians to switch to second‑line options, which may be more expensive or have more side effects. These three connections form the backbone of any effective program.
Beyond medication, vector control plays a supporting role. Insecticide‑treated bed nets, indoor residual spraying, and environmental management lower the number of bites, reducing the number of infections that need treatment. While not a direct part of drug therapy, these measures cut the overall disease burden, making treatment resources stretch further. When resistance spreads, the importance of preventing new cases rises sharply because each bout of malaria becomes harder and costlier to cure.
Understanding resistance trends is a daily task for health workers. Surveillance programs collect data on treatment outcomes, gene mutations, and drug efficacy. This information feeds into national guidelines, which are updated whenever a new resistance hotspot appears. For example, the rise of Kelch13 mutations in Southeast Asia prompted the WHO to recommend alternative partner drugs for ACTs in those zones. Patients benefit from guidelines that reflect real‑world parasite behavior rather than outdated textbook recommendations.
Diagnostic testing also shapes treatment pathways. Rapid diagnostic tests (RDTs) give results in minutes, allowing clinicians to start the right drug promptly. Microscopy remains the gold standard in many referral hospitals because it can differentiate species and parasite density, informing dose adjustments. In remote settings where labs are unavailable, high‑quality RDTs are the primary tool, and training staff to interpret them correctly becomes essential. Misreading a test can either delay needed therapy or expose a patient to unnecessary medication.
Pregnant women and young children require special attention. Certain antimalarials, like doxycycline, are unsafe in pregnancy, so alternatives such as mefloquine or quinine are used instead. Doses are often weight‑based, and follow‑up is crucial to catch any recrudescence early. The World Health Organization recommends intermittent preventive treatment in pregnancy (IPTp) with sulfadoxine‑pyrimethamine wherever resistance is low, highlighting how preventive drug use intersects with treatment strategies.
Travelers to endemic regions also rely on malaria treatment knowledge. Pre‑travel prophylaxis—drugs taken before, during, and after a trip—reduces infection risk, but if a traveler does develop fever abroad, they need to know which drug to seek. Many travel clinics advise carrying a standby treatment, especially for remote trips where medical care is limited. This personal preparedness mirrors the larger public‑health approach: having the right drug on hand when diagnosis confirms infection.
In practice, clinicians juggle multiple factors: species identification, resistance patterns, patient age, pregnancy status, and drug availability. The goal is always a rapid cure with minimal side effects, while also preventing the parasite from adapting to the drugs we use. Staying informed about new drug developments—such as the upcoming tafenoquine regimens for radical cure of P. vivax—helps keep treatment protocols ahead of resistance curves.
Below you’ll find a curated list of articles that dive deeper into each of these areas. Whether you’re looking for a quick guide on ACT dosing, an update on resistance hotspots, or tips for managing malaria in special populations, the collection offers practical insights you can apply right away.
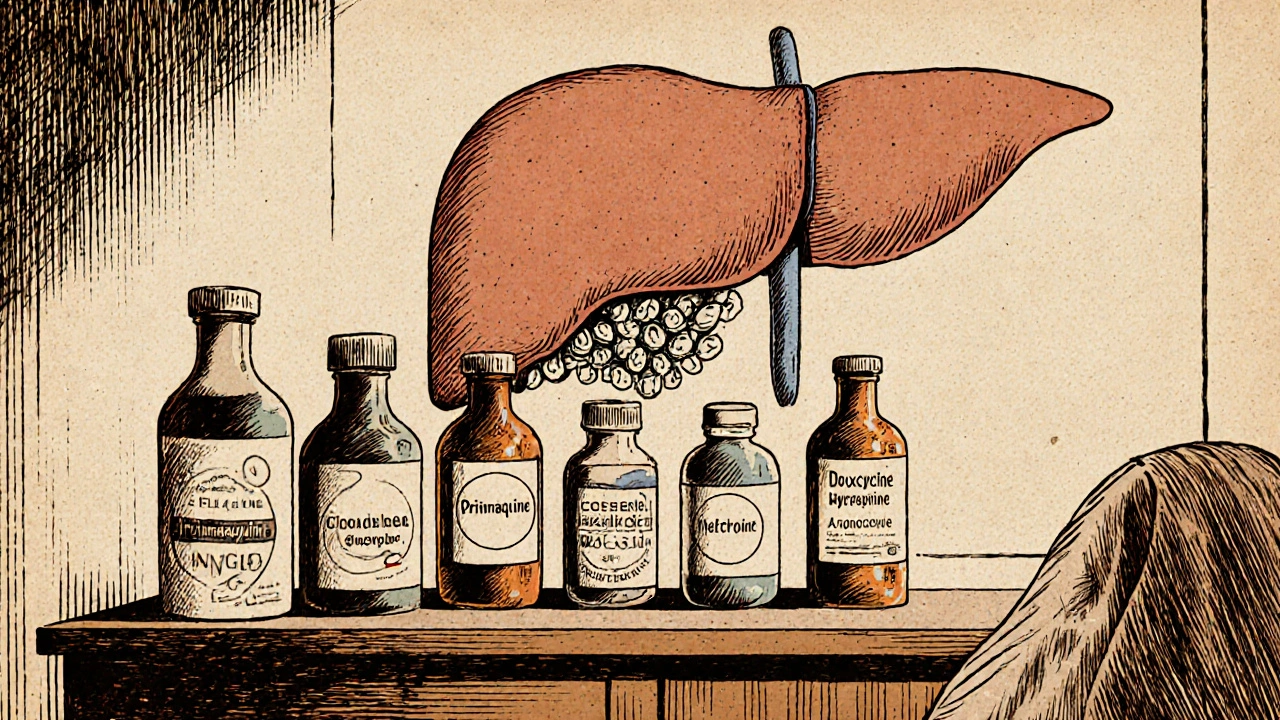
Primaquine vs Other Antimalarials: Detailed Comparison and When to Use Each
A thorough side‑by‑side comparison of primaquine with chloroquine, mefloquine, doxycycline, and atovaquone‑proguanil, covering uses, safety, cost, and how to choose the right antimalarial.