pheochromocytoma prognosis
When talking about pheochromocytoma prognosis, the expected course and survival chances for patients with a catecholamine‑producing adrenal tumor. Also known as PCC outlook, it guides treatment decisions and long‑term monitoring.
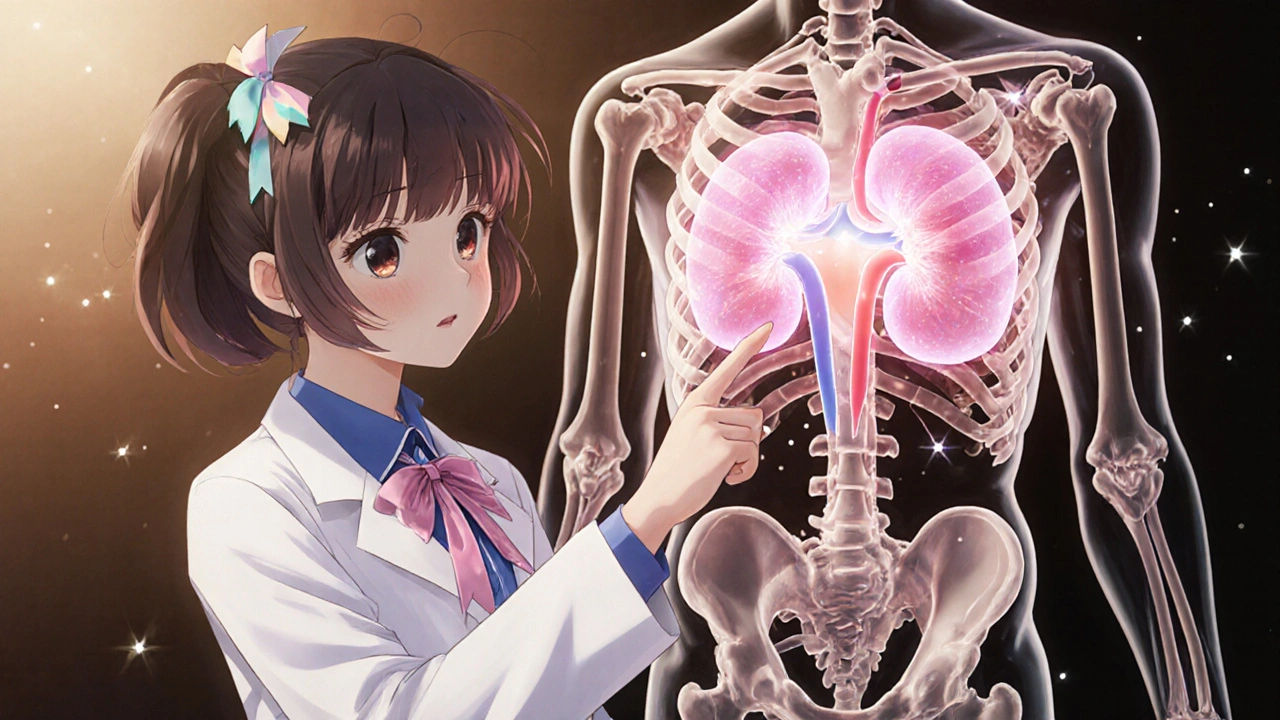
The disease itself, pheochromocytoma, a rare tumor that originates from chromaffin cells of the adrenal medulla and releases excess adrenaline and noradrenaline. Its rarity means many clinicians rely on specialist guidelines, but the core facts stay the same: tumor size, location, and whether it has spread (metastasis) directly shape the prognosis. A small, localized tumor that can be removed surgically usually carries a five‑year survival rate above 90 %. Conversely, extra‑adrenal or metastatic lesions drop that figure dramatically. These facts create the first semantic triple: pheochromocytoma prognosis encompasses tumor size, metastatic status, and surgical resectability. Understanding this link helps patients ask the right questions during consultations.
Key Factors Shaping the Outlook
Modern genetics has added a new layer to the conversation. genetic testing, screening for mutations in genes such as RET, VHL, NF1, and SDHx that predispose individuals to pheochromocytoma can predict both tumor behavior and recurrence risk. Patients with a germline mutation often develop multiple or bilateral tumors, which can lower overall survival if not caught early. The second semantic triple reads: genetic testing influences pheochromocytoma prognosis by identifying high‑risk mutations. Knowing your mutation status also opens doors to targeted surveillance programs, allowing doctors to catch new growths before they become life‑threatening.
When it comes to managing the tumor, surgical resection, the definitive treatment that removes the catecholamine‑producing mass and offers the best chance for cure remains the cornerstone. A minimally invasive laparoscopic approach works for most confined tumors, while open surgery may be required for larger or invasive lesions. Complete removal (R0 resection) creates the third semantic triple: surgical resection improves pheochromocytoma prognosis by eliminating the source of catecholamine excess. Pre‑operative alpha‑blockade is essential to control blood pressure spikes, and postoperative monitoring for biochemical remission confirms success.
Beyond the operating room, the level of catecholamine excess itself matters. Persistent hypertension, arrhythmias, or episodes of severe headache signal ongoing hormone release, which can damage the heart, kidneys, and blood vessels. Effective control of these symptoms before surgery reduces peri‑operative risk and improves long‑term outcomes. In practice, physicians measure plasma free metanephrines or urinary fractionated metanephrines to gauge excess. Lower post‑operative levels usually translate to a better quality of life and a higher probability of staying disease‑free.
Long‑term follow‑up is another piece of the puzzle. Imaging studies—usually MRI or CT—combined with periodic biochemical testing are recommended for at least ten years after resection, especially for those with hereditary forms. Early detection of recurrence allows for repeat surgery or medical management with alpha‑blockers, calcium channel blockers, or newer agents like metyrosine. This ongoing vigilance creates a fourth semantic triple: continuous monitoring supports pheochromocytoma prognosis by catching recurrences early. Patients who stay engaged with their care teams typically enjoy better survival and fewer complications.
Putting all these elements together—tumor characteristics, genetic profile, surgical completeness, hormone control, and vigilant follow‑up—paints a comprehensive picture of what to expect. If you’re reading this, you’ll soon see a curated list of articles that dive deeper into each of these areas, from drug comparisons that matter during pre‑operative preparation to lifestyle tips for managing blood pressure spikes. pheochromocytoma prognosis isn’t a single number; it’s a dynamic story shaped by many factors, and the resources below will help you understand each chapter.
Pheochromocytoma Stages and Grading Explained
Learn how pheochromocytoma is staged and graded, why these systems matter, and how they guide treatment and follow‑up for patients.