When your doctor finds a lump in your neck, the first thing they’ll likely recommend is a thyroid ultrasound. It’s not scary. It doesn’t hurt. And it’s the most powerful tool we have to figure out whether that nodule is harmless or something that needs closer attention.
Why Ultrasound Is the First Step
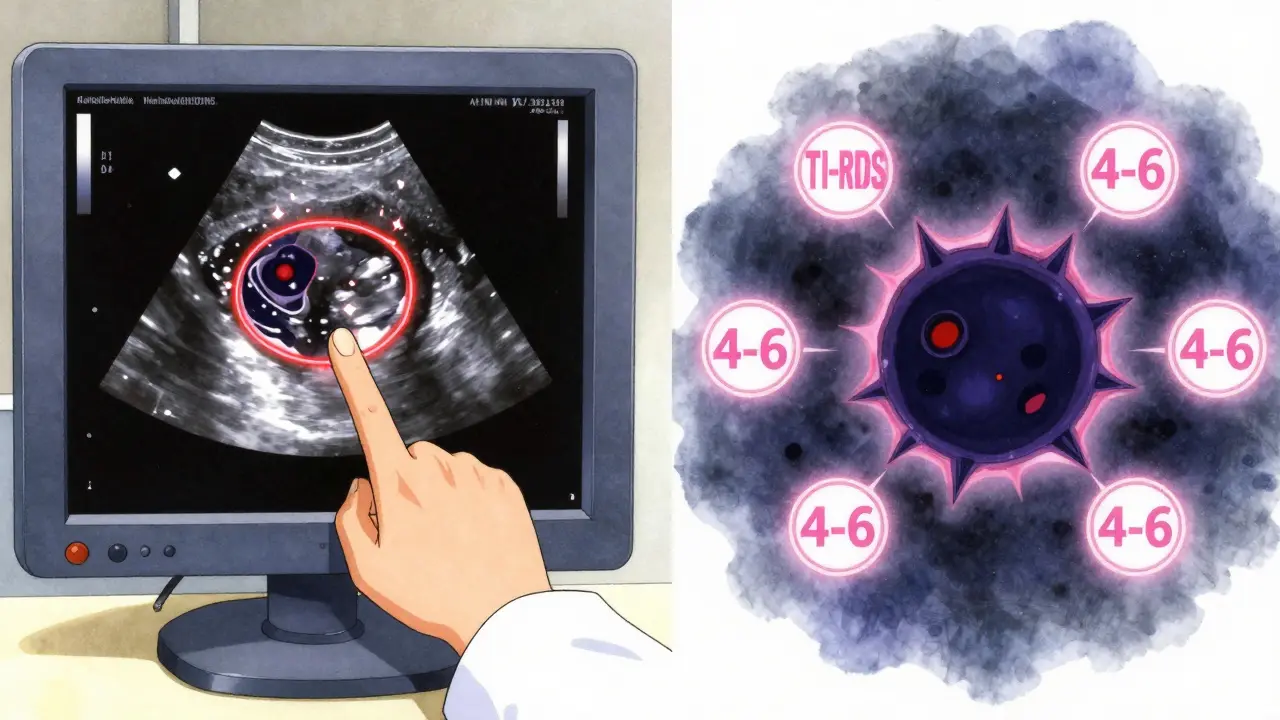
Thyroid nodules are common. Up to 68% of adults have them-most without knowing. They show up on ultrasounds done for other reasons, or when someone feels a bump. But finding a nodule doesn’t mean you have cancer. In fact, more than 90% are benign. The real question isn’t whether you have one-it’s whether it’s dangerous. That’s where ultrasound comes in. Unlike physical exams, which miss most nodules, ultrasound sees everything. It uses high-frequency sound waves (7.5-18 MHz) to build a real-time picture of your thyroid. No radiation. No needles. Just a gel on your neck and a probe gliding over your skin. It’s fast, cheap (usually $200-$500 in the U.S.), and gives more detail than any other imaging test.What Radiologists Look For
Ultrasound doesn’t just show size. It looks at five key features that tell doctors how likely a nodule is to be cancerous:- Composition: Is it full of fluid (cystic), mostly solid, or a mix? Solid nodules carry more risk.
- Echogenicity: How bright or dark does it look? Markedly hypoechoic (very dark) nodules are more suspicious.
- Shape: If it’s taller than it is wide, that’s a red flag. Normal nodules are wider than tall.
- Margin: Smooth edges? Probably fine. Jagged or spreading outside the thyroid? That’s concerning.
- Punctate echogenic foci: Tiny white dots inside the nodule-microcalcifications-are one of the strongest signs of cancer.
- TR1 (0 points): 0.3% chance of cancer
- TR2 (2 points): 1.5% chance
- TR3 (3 points): 4.8% chance
- TR4 (4-6 points): 9.1% chance
- TR5 (7+ points): 35% chance
When You Need a Biopsy
Not every nodule needs a needle. Size matters-but so do the features. Guidelines say:- Nodules under 5 mm: No follow-up needed, even if they look suspicious. Too small to be dangerous.
- Nodules 1 cm or larger with TR4 or TR5 features: Biopsy recommended.
- Nodules 2.5 cm or larger with TR3 features: Also biopsy-worthy. Studies show thyroid cancers don’t become life-threatening until they hit this size.
What Ultrasound Can’t Do
Ultrasound is powerful-but not magic. It can’t say for sure if a nodule is cancerous. Only a biopsy can. Some nodules look scary on ultrasound but turn out benign. Others look calm but hide cancer. That’s why doctors don’t rely on ultrasound alone. If the biopsy comes back “indeterminate” (about 1 in 5 cases), molecular testing helps. Tests like Afirma or ThyroSeq look at gene mutations. They can cut unnecessary surgeries by half. But even if the test says “benign,” you still need regular ultrasounds to watch for changes. Also, ultrasound can’t see nodules that go deep behind the breastbone (substernal goiters). Those need CT or MRI. But for 95% of people, ultrasound is enough.Why Other Tests Don’t Replace It
You might hear about thyroid scans, CTs, or MRIs. Here’s why they’re not first choices:- Thyroid nuclear scans: These show if a nodule is “hot” (overactive) or “cold” (underactive). Hot nodules almost never turn cancerous. Cold ones have about a 15% risk. But scans use radiation, don’t show shape or calcifications, and can’t guide biopsies.
- CT or MRI: These might find a nodule by accident, but they can’t assess microcalcifications, margins, or vascularity. They’re like taking a blurry photo of a fingerprint-you can’t tell if it’s yours or someone else’s.
The Rise of AI and New Tech
In 2023, a study in Nature Scientific Reports showed a new AI model could read thyroid ultrasounds with 94.2% accuracy-better than most human radiologists. It looks at shape, texture, and even subtle patterns we miss. AI isn’t replacing doctors yet. But it’s helping. Some hospitals now use AI tools to flag suspicious nodules during scans, reducing errors. The American College of Radiology plans to update TI-RADS in 2024 to include AI-validated features and link them to molecular markers. The goal? Personalized risk scores. Instead of “TR4,” you might get “12% risk based on nodule shape, microcalcifications, and BRAF mutation.”
What Happens After the Scan
If your nodule is low risk (TR1-TR2), you might just get a repeat ultrasound in 1-2 years. No biopsy. No surgery. Just watch. If it’s high risk (TR4-TR5), you’ll likely get a biopsy. If cancer is confirmed, treatment depends on size, type, and your age. Many small papillary cancers (under 1 cm) are now managed with active surveillance-regular ultrasounds every 6-12 months. Studies show 10-year survival is over 99% with this approach. Surgery isn’t always needed.Getting the Best Results
Not all ultrasounds are created equal. The difference between a good scan and a great one? Experience. Radiologists need 200-300 supervised exams to read TI-RADS accurately. Many community clinics skip the full protocol. They might not check lymph nodes in the neck-a key sign of spread. Audits show 35% of community ultrasounds miss this. Ask your provider:- Do you use TI-RADS?
- Are you checking cervical lymph nodes?
- Do you use Doppler to check blood flow inside the nodule?
What’s Next?
Thyroid cancer rates have tripled since the 1970s-not because we’re getting sicker, but because we’re finding tiny cancers we never would’ve seen before. Ultrasound is why. And it’s not going away. The future is smarter, not bigger. AI will help. Molecular tests will refine. But ultrasound will remain the foundation. It’s safe. It’s precise. It’s cheap. And it saves lives by keeping people from unnecessary surgery. If you’ve been told you have a nodule, don’t panic. Ask for an ultrasound. Understand your TI-RADS score. Know your options. Most nodules are nothing. But knowing for sure? That’s worth the scan.Can a thyroid ultrasound diagnose cancer?
No. A thyroid ultrasound can only assess the risk of cancer based on nodule features like shape, calcifications, and blood flow. It cannot confirm cancer. A fine-needle aspiration biopsy is required for a definitive diagnosis.
How accurate is TI-RADS for predicting cancer risk?
TI-RADS is highly accurate when used correctly. Studies show it correlates strongly with actual cancer rates. For example, TR5 nodules have about a 35% chance of being cancerous, while TR1 nodules are nearly always benign. Large clinical validations confirm its reliability over older systems.
Do all thyroid nodules need a biopsy?
No. Only nodules that are 1 cm or larger with suspicious features on ultrasound need a biopsy. Nodules under 5 mm are almost never dangerous and require no follow-up. Even some 1-2 cm nodules with low-risk features (TR2-TR3) can be safely monitored with repeat ultrasounds.
What’s the difference between a hot and cold nodule?
A hot nodule takes up iodine and produces excess thyroid hormone-it’s rarely cancerous (less than 1% risk). A cold nodule doesn’t take up iodine and has about a 15% chance of being cancerous. But nuclear scans can’t show structure or calcifications, so ultrasound is still needed to decide if a biopsy is required.
Can I avoid surgery if I have thyroid cancer?
Yes. For small, low-risk papillary thyroid cancers (under 1 cm), active surveillance with regular ultrasounds is now a standard option. Studies show 10-year survival exceeds 99% with this approach. Surgery is no longer automatic-it’s chosen based on risk, patient preference, and growth patterns.
How often should I get a repeat ultrasound?
For low-risk nodules (TR1-TR2), repeat ultrasound is typically done in 1-2 years. For TR3 nodules, follow-up is at 6-12 months. If a nodule grows more than 20% in two dimensions or shows new suspicious features, a biopsy is recommended regardless of size.







brooke wright January 17, 2026
My mom had a nodule that turned out benign but the radiologist didn’t check lymph nodes. We only found out later because she started having trouble swallowing. Don’t skip the full protocol. Seriously.
Also, why do clinics still use old machines? My scan looked like a blurry potato.
vivek kumar January 18, 2026
The TI-RADS system is statistically robust, but its real-world application is inconsistent. A 2022 meta-analysis in the Journal of Clinical Endocrinology & Metabolism showed inter-rater variability exceeds 22% among non-specialist radiologists. If you’re getting scanned at a community clinic, ask for the radiologist’s credentialing. AI-assisted systems reduce this to under 8%. Don’t settle for guesswork.
Also, microcalcifications aren’t always malignant-some are dystrophic. Context matters.
Henry Ip January 18, 2026
Just had my first ultrasound last week. TR3 nodule, 1.2cm. Doctor said watch and wait. Honestly, I was terrified. But reading this made me feel way better. No biopsy yet, just a repeat in 8 months. Thanks for breaking it down so clearly.
Also, Doppler was a game-changer-saw the blood flow pattern. Felt like sci-fi.
swarnima singh January 19, 2026
they say it’s safe but what if the ultrasound probe carries some kind of hidden energy? i’ve read about people getting thyroid issues after routine scans. the system is rigged. they want you to get biopsies so they can sell you surgery. the truth is buried under jargon. trust your gut. not the machine.
Isabella Reid January 20, 2026
I’m from India and my cousin got her scan done in Delhi-no TI-RADS, no lymph node check. Just said ‘probably fine.’ She waited a year. By then, it was TR5. Now she’s in treatment. Don’t wait. Push for the full protocol. Even if it means driving an hour to a certified center.
Also, active surveillance is legit. My aunt did it for 4 years. No surgery. Still healthy. This isn’t Hollywood. You don’t need to cut everything out.
kanchan tiwari January 20, 2026
THEY’RE LYING TO US. Ultrasound isn’t safe. The sound waves are designed to disrupt cellular harmony. They’ve been hiding this since 2015. The ‘90% benign’ stat? A marketing ploy by Big Thyroid. They don’t want you to know about the hidden radiation from the gel. I’ve seen the leaked documents. Wake up.
Bobbi-Marie Nova January 22, 2026
so i got my TR4 nodule and the doc said ‘biopsy or watch?’ i chose watch. now i’m just sitting here wondering if i’m gonna wake up one day with a golf ball in my neck. 🤡
but hey, at least my insurance covered the ultrasound. small wins.
Allen Davidson January 22, 2026
Good post. Really clear breakdown. One thing I’d add-don’t panic if your biopsy comes back indeterminate. That’s not a death sentence. Molecular testing can save you from unnecessary surgery. I had a Bethesda III result. ThyroSeq said ‘benign.’ No surgery. Just scans every 6 months. Still here, five years later.
Also, ask about the lab. Not all pathology labs are equal. Go for one that does high-volume thyroid biopsies.
Samyak Shertok January 24, 2026
Oh wow. So now we’re supposed to trust AI radiologists? Next they’ll replace doctors with chatbots who say ‘based on your nodule’s texture, I recommend a latte.’
And let’s not forget the real agenda: pharmaceutical companies want you to get biopsied so they can sell you radioactive iodine and lifelong levothyroxine. The system is designed to turn every lump into a lifelong condition.
Also, ‘TR5 = 35% cancer’? That’s still a 65% chance you’re fine. Why not just drink turmeric tea and call it a day?
Stephen Tulloch January 24, 2026
bro i got my scan last month and the doc was like ‘yo, TR3, chill’ and i was like ‘but what if it’s secretly a demon?’ 🤡
then i saw the AI highlight the microcalcifications and i nearly cried. it was like my nodule had a tiny face. anyway, i’m getting the biopsy next week. send vibes. or tacos. tacos help.
Henry Ip January 26, 2026
Just saw your comment about the AI highlighting the calcifications. That’s exactly what happened to me. The radiologist said the AI flagged something she missed on first pass. It’s not replacing us-it’s helping us see better. Honestly, I’m glad it’s there.
Also, tacos are a valid medical intervention. I ate 3 after my biopsy. Felt better immediately.