When you’ve been on the same psychiatric medication for months-or years-it stops feeling like a drug. It feels like part of you. The calm after the storm. The quiet in your head. Then, without warning, your doctor says: switch.
It’s not always your choice. Insurance changes. Generic substitutions. Lack of response. Cost. Suddenly, the pill you relied on is gone. And in its place? Something unfamiliar. Something untested. And for many, the psychological fallout is worse than the original symptoms.
Why Switching Feels Like Losing Yourself
People don’t just stop taking medication. They stop taking who they’ve become on it.
A 2023 study in Frontiers in Psychiatry tracked how patients experienced medication changes over time. Nearly all of them-100%-described a phase they called “loss of self.” That’s not dramatic language. That’s clinical observation. Patients reported feeling like strangers in their own bodies. Like their emotions had been muted, then suddenly turned back on at full volume. Some said they cried for no reason. Others couldn’t feel anything at all.
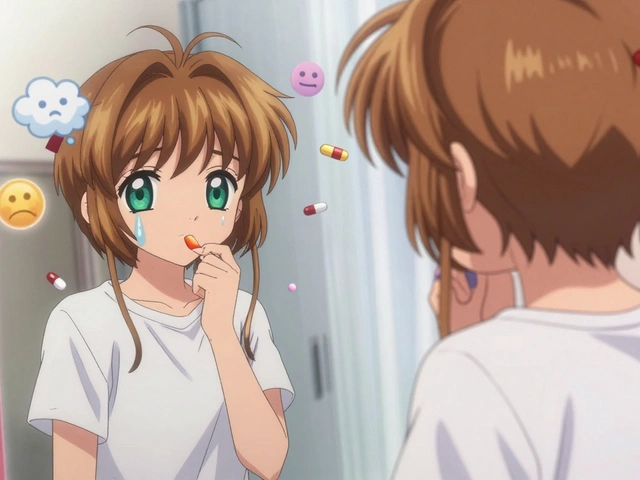
One woman on Reddit, u/MedSwitchSurvivor, wrote: “I switched from brand sertraline to generic. Three weeks later, I didn’t recognize my own face in the mirror. I was numb. Then I was terrified. I hadn’t had a panic attack in two years. Suddenly, they came daily.”
This isn’t rare. The National Alliance on Mental Illness (NAMI) surveyed over 1,800 people in 2022. Sixty-three percent said they experienced psychological distress during a medication switch. Forty-one percent saw their anxiety spike. Thirty-seven percent had thoughts of suicide. These aren’t side effects. These are psychological ruptures.
The Hidden Trap: Generic Substitutions
Most switches aren’t planned. They’re forced.
Insurance companies push generics. Pharmacies substitute. Patients often don’t even know they’ve been switched until they feel off. And when they do, doctors sometimes dismiss it: “It’s the same drug.”
But it’s not.
A 2019 review by Dr. Pierre Blier found that 68% of problematic switches happened between different generic versions-not between brand and generic. Why? Because generics aren’t identical. They have different fillers, coatings, release mechanisms. For drugs with narrow therapeutic windows-like SSRIs, antipsychotics, and mood stabilizers-those tiny differences matter.
One patient switched from one generic paroxetine to another. Within days, he had electric-shock sensations in his head, dizziness, and a return of severe depression. He later learned his pharmacy had changed suppliers. No one told him. No one asked how he felt.
And here’s the cruel twist: bioequivalence standards don’t account for psychological stability. The FDA says two drugs are “equivalent” if they have the same blood levels. But your brain doesn’t care about blood levels. It cares about consistency. It remembers the rhythm. When that rhythm breaks, your nervous system panics.
Why Some Switches Work-And Others Destroy Progress
Not all switches are disasters. Some people feel better.
In the same NAMI survey, 28% reported improved mood after switching-usually when they moved from a drug that caused brain fog or weight gain to one that didn’t. A man on PatientsLikeMe switched from fluoxetine to escitalopram and said, “I finally felt like I could think again.”
But the difference? Control. Clarity. Communication.
Successful switches happen when:
- The patient is involved in the decision
- The change is gradual-cross-tapering over 3 to 4 weeks
- The doctor explains why the switch is happening
- Monitoring is frequent, especially in the first two weeks
One 2021 meta-analysis found that tapering schedules matched to a drug’s half-life cut withdrawal symptoms by 30%. Paroxetine (21-hour half-life) needs a slower taper than fluoxetine (96-hour half-life). Yet most primary care providers don’t know this.
According to the American Academy of Family Physicians, 61% of family doctors say they lack proper training in cross-tapering. That means most switches are rushed. Done in 7 to 10 days. With no follow-up. And patients are left to suffer alone.

The Trust Crisis
Psychiatrists know this. But primary care doctors? They’re overwhelmed.
Eighty-five percent of primary care providers now manage long-term mental health meds. But only 22% of family medicine residencies teach medication switching protocols. That’s a massive gap.
And when patients feel unheard, trust breaks.
A Psych Central poll in March 2023 found that 74% of users felt less confident in their treatment after an unplanned switch. One man said: “I trusted my doctor. Then they switched me without asking. I didn’t feel like a patient. I felt like a number.”
Dr. K. N. Roy Chengappa calls this “therapeutic alliance erosion.” It’s not just about the drug. It’s about the relationship. When a switch happens without explanation, patients feel betrayed. Like their mental health wasn’t taken seriously. That trauma can last longer than any withdrawal symptom.
Genes, Income, and the Hidden Inequality
Not everyone experiences switching the same way.
King’s College London studied over 40,000 people and found that those with higher polygenic risk scores for depression recovery failure were 23% more likely to need a switch. Genetics matter. But so does money.
UK Biobank data showed patients earning under $30,000 a year were 33% more likely to have negative psychological outcomes after a switch than those earning over $75,000. Why? Access. Support. Time.
People with more resources can afford to wait. They can see specialists. They can request brand-name drugs. They can take time off work to monitor symptoms. They can afford therapy to process the emotional fallout.
Those without? They get the fastest, cheapest option. And they pay the price in panic attacks, insomnia, and relapse.
And it’s not just about the drug. It’s about the system.

What You Can Do-Before, During, and After a Switch
If you’re facing a switch, here’s how to protect your mental health:
- Ask why. Is this for cost? Efficacy? Insurance? Demand clarity. Don’t accept “it’s just a generic” as an answer.
- Request a cross-taper. Never stop cold. Ask for a 3- to 4-week transition where the old drug is slowly reduced while the new one is introduced.
- Know your drug’s half-life. Paroxetine? Escitalopram? Venlafaxine? These have short half-lives. They need slower tapers. Fluoxetine? Longer. Can be tapered faster. Ask your pharmacist.
- Track your symptoms. Use a simple journal: mood, sleep, anxiety, physical sensations. Take it to every appointment.
- Insist on follow-ups. Schedule check-ins every week for the first month. Don’t wait until you’re in crisis.
- Speak up if you feel worse. If you feel like you’re losing yourself, say it. Write it down. Send an email. This is your brain. Your life.
And if your doctor dismisses you? Find someone who won’t. Mental health care isn’t one-size-fits-all. Your stability matters more than a pharmacy’s profit margin.
The Future Is Changing-But Slowly
The FDA is launching a new surveillance system in 2024 to track psychological outcomes from medication switches across 25 million patient records. That’s a start.
Companies like Pear Therapeutics now offer apps that monitor symptoms during transitions. In trials, they reduced hospitalizations by 27%.
But the real fix? Training. Policy. Respect.
Psychiatric medications aren’t like antibiotics. You don’t just kill a bug and feel better. These drugs reshape your brain chemistry. Your identity. Your sense of safety. Switching them isn’t a administrative task. It’s a psychological event.
And until the system treats it that way, people will keep feeling broken-not because their meds failed, but because the system forgot they’re human.








Saket Modi December 1, 2025
bro i switched from sertraline to some generic crap and woke up crying for no reason for 3 weeks. my dog even avoided me. 😭
Chris Wallace December 2, 2025
I’ve been on the same SSRI for seven years. When they switched me without warning, it felt like someone rewired my brain with duct tape. The numbness came first, then the panic. I didn’t realize how much I’d come to rely on that quiet. It wasn’t just the drug-it was the version of me that existed inside it. And now? I’m just... guessing who I am again.
william tao December 3, 2025
The notion that pharmaceutical equivalence equates to clinical equivalence is a dangerous fallacy. The FDA's bioequivalence criteria are statistically derived from population-level pharmacokinetics-utterly inadequate for neurochemical individuality. One must acknowledge that the central nervous system is not a hydraulic system; it is a dynamic, adaptive network. Disruption of pharmacodynamic consistency induces neuroplastic dissonance. This is not anecdotal. It is neurobiological.
Sandi Allen December 5, 2025
THIS IS WHY THEY WANT YOU DEPRESSED!! The pharma companies and insurance bots are in cahoose!! They want you hooked on the new drug after they break you with the switch!! And the doctors? They’re paid by the pill-pushers!! They don’t care if you cry yourself to sleep at 3am!! They just want you to sign the consent form and shut up!! THEY’RE KILLING US SLOWLY AND NO ONE WILL LISTEN!!
John Webber December 6, 2025
i switched meds once and i swear i felt like i was dreaming. like my brain was on mute then someone turned the volume to 11. i didnt even know i was crying until my roommate asked if i was ok. i just sat there. i dont even remember the name of the new pill. i just know i hated it. and no one listened.
Shubham Pandey December 6, 2025
Generic switch = bad. Just say no.
Elizabeth Farrell December 7, 2025
I want to say thank you for writing this. I’ve been silent about my own switch for over a year. I went from escitalopram to a generic version, and I didn’t realize how much I’d been holding onto until it was gone. The first week, I felt like I was underwater. I stopped recognizing my own laugh. But I kept a journal. I asked for a cross-taper. I found a therapist who actually listened. It took months, but I’m back. Not the same, maybe-but safer. You’re not alone. And your feelings? They’re valid. Always.
Sheryl Lynn December 9, 2025
The tragedy isn’t the pharmacokinetic variance-it’s the bourgeois indifference. We’ve reduced the sacred act of neurochemical recalibration to a spreadsheet optimization. A mere line item in the cost-benefit analysis of managed care. One’s psyche is not a commodity to be bartered in the pharmacy queue. The true pathology lies not in the drug, but in the system that commodifies consciousness.
Paul Santos December 10, 2025
Honestly, it’s like your brain develops a synaptic memory of the drug’s rhythm. Switch it out and your limbic system throws a tantrum. 🤯 It’s not placebo-it’s neuro-attachment. The body remembers. And the system? Doesn’t care. Pharma’s got their bioequivalence boxes ticked. But your soul? Nah. That’s not in the FDA’s database. 😅
Eddy Kimani December 12, 2025
This is fascinating from a neuropharmacological standpoint. The half-life mismatch is critical-especially with short-half-life agents like paroxetine. The synaptic serotonin reuptake transporter occupancy decays rapidly, triggering a compensatory downregulation cascade. Without tapering, you induce a transient hyper-serotonergic rebound followed by hypofunction. It’s not 'in your head'-it’s a documented neuroadaptive response. We need standardized taper protocols based on pharmacodynamic half-lives, not calendar days.
Chelsea Moore December 12, 2025
I switched and I LOST MYSELF for 11 weeks. I didn’t eat. I didn’t talk. I stared at the wall. My mom cried when she saw me. My therapist said I was ‘adjusting.’ ADJUSTING?? I was a ghost. And now they want to do it again? NO. I’M NOT A LAB RAT. I’M A PERSON. AND I’M TIRED OF BEING TREATED LIKE A NUMBER IN A DATABASE!!
John Biesecker December 13, 2025
you ever feel like your brain is a song and the med is the melody? you get used to the tune... then someone changes the key and you just... stop singing. i dont know why i cried for three days straight after the switch. i just felt like i lost my favorite blanket. 🤕
Genesis Rubi December 14, 2025
America needs to stop letting big pharma control our brains. We’re not China. We’re not Canada. We’re the land of the free-so why are we letting insurance companies decide what our minds feel? This is why I’m voting for Medicare for All. No more generic swaps. No more silent suffering. We deserve better.
Doug Hawk December 15, 2025
I’ve seen this in clinical practice. The real issue isn’t the drug-it’s the lack of monitoring. Patients are discharged with a script and told to ‘call if something’s wrong.’ But when your nervous system is in chaos, you don’t know what’s ‘wrong.’ You just feel broken. We need mandatory 7-day and 14-day follow-ups after any switch. Simple. Cost-effective. Life-saving.
william tao December 16, 2025
The empirical data presented here is compelling, yet the underlying assumption-that psychiatric medication serves as an ontological anchor-is itself a product of biopsychological reductionism. One must interrogate whether the 'self' is a stable entity at all, or merely a narrative constructed in the feedback loop between neurochemistry and social expectation. The crisis of identity following a switch may not be a failure of pharmacology, but a revelation of the fragility of the ego.