Chronic Diarrhea: Causes, Symptoms, and Treatment Options
When dealing with chronic diarrhea, frequent watery stools lasting more than four weeks. Also known as persistent diarrhea, it often signals an underlying issue and can disrupt daily life.
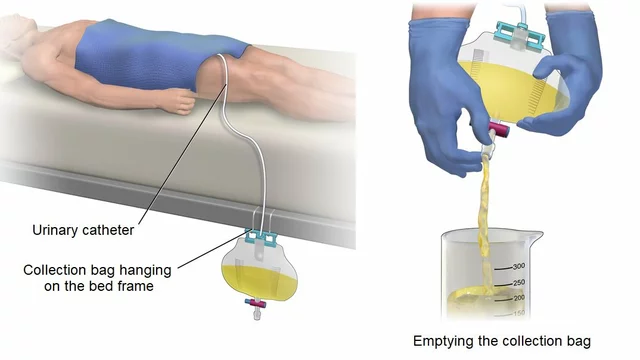
Understanding the condition means looking at the main players that can trigger or relieve it. antibiotics, medications that kill or inhibit bacteria are a double‑edged sword: they can cause diarrhea by disturbing gut flora, yet they also treat bacterial infections that lead to diarrhea. probiotics, live microorganisms that restore a healthy gut balance help rebuild that flora after a course of antibiotics or an infection. oral rehydration solution, a blend of salts and sugars that replaces lost fluids prevents dehydration, a frequent danger when stools are watery for weeks. Finally, inflammatory bowel disease, a group of chronic inflammatory conditions of the digestive tract is a common long‑term cause of persistent loose stools. In short, chronic diarrhea encompasses prolonged watery bowel movements, requires proper diagnosis, and can be influenced by antibiotics, helped by probiotics, managed with oral rehydration, and sometimes stems from inflammatory bowel disease.
Understanding the Roots of Persistent Loose Stools
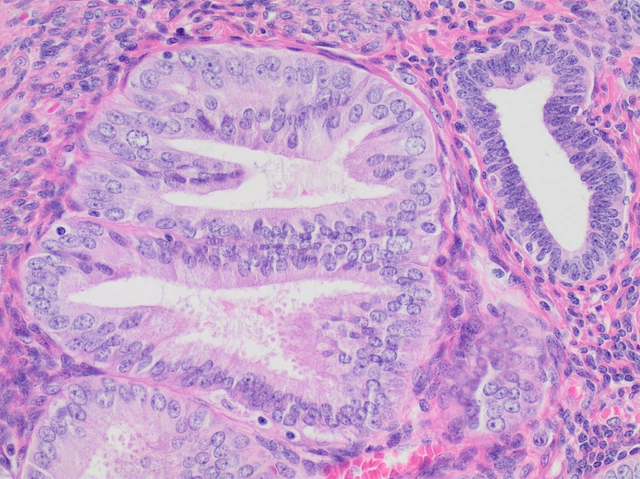
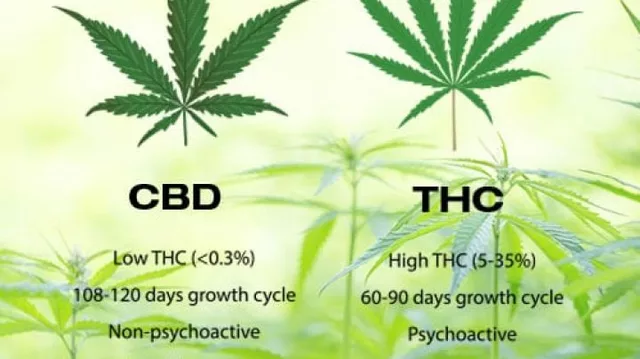
There are many ways chronic diarrhea can start. Infections from bacteria like Clostridioides difficile, parasites, or viruses often follow a recent antibiotic course, because the drug wipes out good bacteria and lets the harmful ones thrive. Food intolerances—lactose, fructose, or gluten—can also cause ongoing symptoms if the offending foods are not identified. Medication side effects, especially from pills that affect the gut (like certain antacids or chemotherapy agents), add another layer. Chronic conditions such as chronic diarrhea linked to inflammatory bowel disease (Crohn’s disease or ulcerative colitis) demand long‑term management, while malabsorption syndromes (like celiac disease) keep the digestive system from pulling nutrients, leading to watery stools. The common thread is that each cause either disrupts the gut’s normal absorption or alters the bacterial environment, and recognizing which factor is at play is key to stopping the cycle.
Managing the condition starts with staying hydrated and choosing a gut‑friendly diet. Drinking oral rehydration solution or a simple mix of water, salt, and sugar keeps electrolyte levels stable. A low‑fiber, bland diet—think bananas, rice, applesauce, toast—gives the intestines a break while you figure out the culprit. Over‑the‑counter anti‑diarrheal agents such as loperamide can provide short‑term relief, but they shouldn’t mask serious underlying problems. Probiotic supplements, especially those containing Lactobacillus and Bifidobacterium strains, are useful after antibiotics or infections to rebalance gut flora. If symptoms persist beyond a few days, stool tests, blood work, and possibly a colonoscopy become essential to rule out infections, inflammatory bowel disease, or other chronic disorders. The right combination of hydration, diet, targeted medication, and, when needed, specialist care will bring you back to normal bowel function. Below, you’ll find a curated set of articles that dive deeper into specific causes, drug comparisons, and practical tips for handling chronic diarrhea and related gut health issues.
Massage Therapy Benefits for Chronic Diarrhea Relief
Discover how massage therapy can calm the gut, reduce inflammation, and ease chronic diarrhea symptoms. Learn the best techniques, scientific evidence, and practical tips for safe, effective treatment.