When you pick up a prescription for a generic drug, you’re not getting a cheaper version of medicine-you’re getting the same medicine. The FDA requires generic drugs to match brand-name drugs in every way that matters: active ingredient, strength, dosage form, and how your body absorbs it. This isn’t just a suggestion. It’s the law. And the system behind it is one of the most rigorously tested in all of healthcare.
What Makes a Generic Drug Really Equivalent?
Two things make a generic drug legally and medically the same as its brand-name counterpart: pharmaceutical equivalence and bioequivalence. Pharmaceutical equivalence means the generic has the exact same active ingredient, in the same amount, delivered the same way-whether it’s a pill, injection, or inhaler. The shape, color, or taste? Those can be different. Inactive ingredients like fillers or dyes? Those can vary too. But the medicine that actually treats your condition? That has to be identical.
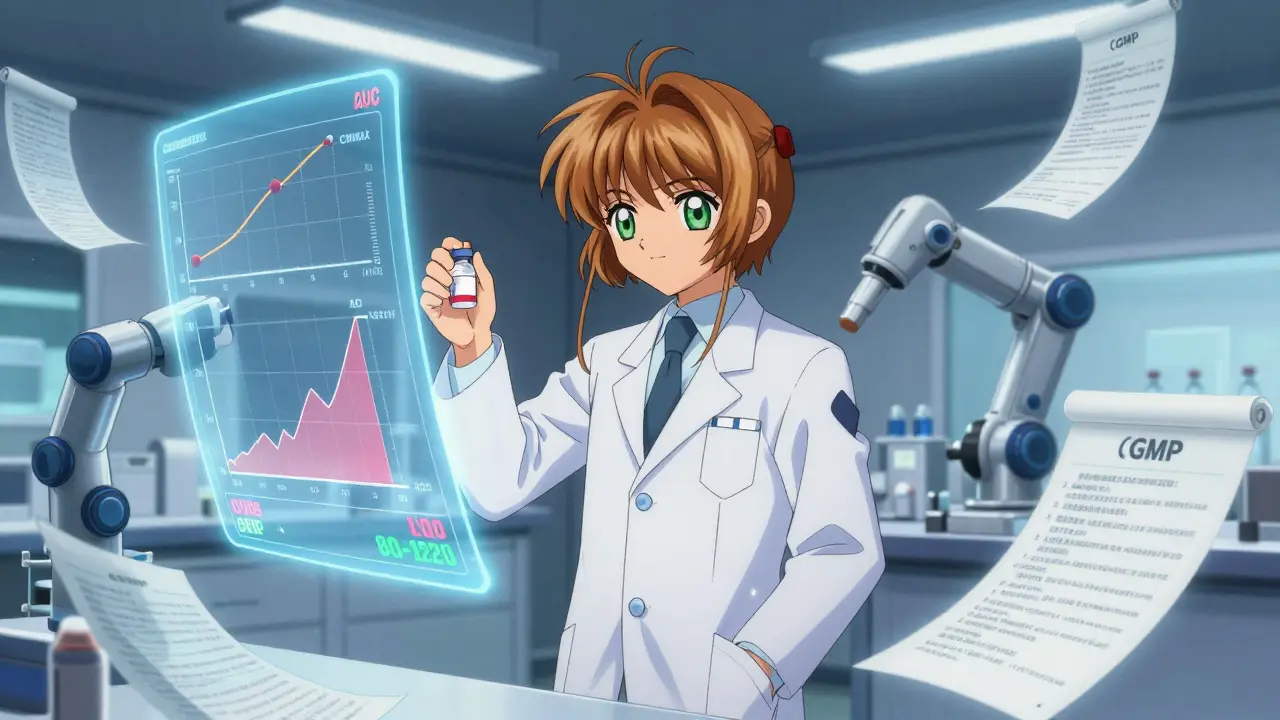
Bioequivalence is where things get technical-and critical. It means your body absorbs the generic drug at the same rate and to the same extent as the brand-name version. The FDA doesn’t just trust manufacturers’ claims. They require real-world testing. For most small-molecule generics, this means a study with 24 to 36 healthy volunteers. Blood samples are taken over time to measure two key metrics: Cmax (the highest concentration in the blood) and AUC (how much of the drug is absorbed over time). The results must fall within 80% to 125% of the brand-name drug’s values. If they don’t, the generic doesn’t get approved.
How the FDA Ensures Consistent Quality
Manufacturing a generic drug isn’t like copying a recipe. It’s like rebuilding a precision engine. Every step-from sourcing raw materials to packaging the final product-must follow Current Good Manufacturing Practices (cGMP), which are legally binding rules under 21 CFR Parts 210 and 211. These rules cover everything: how materials are stored, how equipment is cleaned, how each batch is tested, and how records are kept. There’s no room for guesswork.
The FDA inspects about 3,500 manufacturing sites every year-some in the U.S., many overseas. These aren’t surprise visits. They’re planned, thorough, and often unannounced. The agency checks for contamination risks, equipment calibration, data integrity, and whether workers follow written procedures. And here’s something many people don’t know: about half of all generic drugs in the U.S. are made by the same companies that make the brand-name versions. Often, they’re made in the same factories, on the same lines. The only difference is the label.
The ANDA Process: How Generics Get Approved
To get a generic drug on the market, a company submits an Abbreviated New Drug Application (ANDA). It’s called “abbreviated” because it doesn’t require repeating the full clinical trials done for the original drug. Instead, it focuses on proving equivalence through chemistry, manufacturing, and bioequivalence data. But don’t mistake “abbreviated” for “easy.” The FDA reviews every detail.
The review process takes about 10 months for a complete application under current timelines set by the Generic Drug User Fee Amendments (GDUFA). But it’s not always smooth. In 2022, the FDA issued 478 complete response letters-essentially, “we need more info” notices-while approving 892 original ANDAs. Many applications get rejected or delayed because of manufacturing flaws, inconsistent testing methods, or missing stability data.
Stability testing is a big part of that. Generics must prove they’ll stay effective and safe for their entire shelf life-usually 12 to 24 months. Manufacturers run accelerated tests (like exposing the drug to 40°C and 75% humidity for six months) and long-term tests under normal storage conditions. If the drug breaks down too fast or changes chemically, it’s rejected.
Complex Generics: When It’s Not Just a Pill
Not all drugs are created equal. A simple tablet is easy to copy. But what about an inhaler that delivers medicine deep into the lungs? Or a topical cream that needs to penetrate skin at just the right rate? Or a long-acting injection that releases drug slowly over weeks? These are complex generics, and they’re much harder to replicate.
For these, the FDA requires more than just blood tests. They need advanced physical and chemical analysis to prove the generic matches the original in structure, particle size, spray pattern, or release profile. This is called “Q3 sameness”-meaning the generic must be the same in quality, performance, and characteristics. As of 2023, the FDA has issued over 2,100 product-specific guidances for complex generics, covering more than 1,500 different drugs. In 2023 alone, they released 27 new guidances to help manufacturers meet these higher standards.
Some experts, like former FDA official Dr. Charles Ganley, admit that even with these tools, proving equivalence for complex products remains challenging. For example, two inhalers might have the same active ingredient and dose, but if the particle size distribution differs slightly, the drug may not reach the same part of the lung. That’s why the FDA has invested $15.7 million into research for better testing methods and hosts public workshops with scientists and industry experts to solve these problems.

Why Generics Save Billions-and Still Work
Generic drugs make healthcare affordable. In 2022, they saved the U.S. healthcare system $37 billion. They account for more than 90% of all prescriptions filled, but only about 23% of total drug spending. That’s the power of competition.
And they’re trusted. A 2022 Consumer Reports survey of 1,200 Americans found 89% were satisfied with generic medications, and 62% actively chose them to save money. Major medical groups like the American Medical Association and the American Academy of Family Physicians have publicly backed generics for over a decade.
But there are exceptions. Some drugs have a narrow therapeutic index-meaning even small changes in blood levels can cause problems. Levothyroxine, used for thyroid conditions, is one. A 2021 JAMA study found that 12.3% of patients who switched between different generic versions experienced thyroid hormone fluctuations that required dose adjustments. For drugs like warfarin or certain seizure medications, doctors sometimes stick with brand names out of caution.
Still, for the vast majority of patients, generics are safe, effective, and identical. A 2023 Reddit thread with over 1,400 responses from patients and pharmacists showed 83% reported no difference between brand and generic versions. The few who did notice changes often couldn’t pinpoint why-sometimes it was the pill’s size or coating, not the medicine itself.
What You Should Know Before Taking a Generic
If you’re prescribed a generic, you’re getting a drug that’s been tested as thoroughly as the brand-name version. The FDA doesn’t cut corners. They require the same quality controls, the same manufacturing standards, and the same proof of effectiveness.
Don’t assume a cheaper price means lower quality. The cost difference comes from marketing, patents, and brand loyalty-not from inferior ingredients or sloppy production.
For most people, switching to a generic is safe and smart. If you’re on a narrow therapeutic index drug and notice changes in how you feel after switching, talk to your doctor. But don’t avoid generics out of fear. The science is clear: FDA-approved generics work the same way, at the same dose, with the same safety profile.
The system isn’t perfect. Complex drugs are still a challenge. Some batches may have minor variations. But the oversight is constant, the standards are strict, and the results speak for themselves. Over 20,000 generic products are approved in the U.S. today. Millions of people rely on them every day. And the FDA keeps watching-because your health isn’t a cost-cutting experiment. It’s a promise.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same high standards for safety, strength, purity, and stability as brand-name drugs. They undergo the same manufacturing inspections, quality controls, and testing protocols. The only difference is the price-most generics cost 80% to 85% less.
Why do some generics look different from the brand-name version?
U.S. law allows generic manufacturers to change the color, shape, size, or flavor of a drug, as long as the active ingredient and dosage are identical. These differences are cosmetic and have no effect on how the drug works. You might notice a different pill shape, but the medicine inside is the same.
Can I switch between different generic versions of the same drug?
For most drugs, yes. All FDA-approved generics for the same drug must meet bioequivalence standards. But for drugs with a narrow therapeutic index-like levothyroxine, warfarin, or certain seizure medications-switching between different generic versions may cause small changes in blood levels. If you’re on one of these, talk to your doctor before switching brands.
Do generic drugs take longer to work than brand-name drugs?
No. Generic drugs must reach the same level in your bloodstream at the same rate as the brand-name version. The FDA requires bioequivalence testing to prove this. If a generic absorbed slower or faster, it would be rejected. You won’t feel a delay in effect.
Are generic drugs made in the same factories as brand-name drugs?
Yes, often. About half of all generic drugs in the U.S. are manufactured by the same companies that make the brand-name versions. Many are made in the same facilities, sometimes on the same production lines. The FDA inspects all these sites equally, regardless of whether they make brand or generic drugs.
How does the FDA test generic drugs before approval?
The FDA reviews chemistry data, manufacturing processes, and bioequivalence studies. For most drugs, this includes clinical trials with 24-36 healthy volunteers to measure how the drug is absorbed. For complex drugs like inhalers or creams, they use advanced physical and chemical tests to match the original product’s structure and performance. Every batch must also pass identity, strength, and purity tests before release.
What happens if a generic drug fails FDA testing?
If a generic fails to meet bioequivalence, stability, or manufacturing standards, the FDA issues a complete response letter and denies approval. The company must fix the issue and resubmit. In 2022, nearly half of all ANDA applications required revisions before approval. The FDA doesn’t approve drugs that don’t meet the standard-no exceptions.
Is it true that some generics are made overseas?
Yes, about 80% of generic drug ingredients and 40% of finished products come from overseas, mostly from India and China. But the FDA inspects foreign factories just like U.S. ones. In 2023, over 1,000 inspections were conducted in India alone. If a facility fails inspection, the FDA can block imports until problems are fixed.
Why do some people say generics don’t work as well?
Most of the time, it’s not the drug-it’s the placebo effect, or changes in inactive ingredients affecting how the pill feels in the mouth or how quickly it dissolves. For a small number of patients on narrow therapeutic index drugs, switching between generic manufacturers can cause minor fluctuations. But these cases are rare, and doctors can manage them. The overwhelming majority of patients experience no difference.
How often does the FDA check on generic drug manufacturers?
The FDA inspects about 3,500 manufacturing sites each year-both domestic and foreign. These inspections are unannounced and cover everything from raw materials to finished product testing. Facilities that fail inspections can be shut down or blocked from selling drugs in the U.S. The agency also monitors post-market reports for adverse events linked to generics, just like with brand-name drugs.










John McGuirk January 23, 2026
They say generics are the same, but have you ever seen the FDA’s inspection reports? Half the time, they’re just rubber-stamping stuff from factories in India where workers are paid pennies. And don’t get me started on the ‘same factory’ lie - same building, sure. Same line? Nah. They clean the machines with a rag and pray. I’ve seen the leaks. This ain’t science, it’s a corporate shell game.
Jamie Hooper January 23, 2026
okay so i took my generic adderall and it felt like someone poured concrete in my brain… then i switched back to brand and boom, i could actually think again?? 🤷♂️ maybe the ‘bioequivalent’ stuff is just a fancy word for ‘close enough for government work’
Izzy Hadala January 23, 2026
The bioequivalence criteria of 80–125% AUC and Cmax is statistically robust and aligned with international standards (WHO, EMA). The variability window is derived from pharmacokinetic modeling and accounts for inter-individual metabolic differences. To suggest equivalence is unscientific is to misunderstand the nature of pharmacokinetic variability, not the regulatory framework.
Sushrita Chakraborty January 24, 2026
In India, we produce over 50% of the world’s generic medicines - and yes, we follow cGMP, too. Our inspectors are trained by the FDA, and our labs are ISO-certified. It’s not about where it’s made - it’s about whether the standards are upheld. The FDA doesn’t discriminate by country. It discriminates by compliance.
Sawyer Vitela January 24, 2026
80-125% range is a joke. That’s a 45% swing. If your blood level of warfarin drops 20%, you clot. If it spikes 20%, you bleed. That’s not equivalence. That’s Russian roulette with your life.
Shanta Blank January 25, 2026
They call it ‘generic’ like it’s a discount brand of toilet paper. But this isn’t Charmin - this is your heart, your brain, your damn thyroid. I had a seizure because I switched generics. Now I pay $180 a month for the brand because I refuse to gamble with my nervous system. The FDA’s ‘same’ is a lie wrapped in a spreadsheet.
Dolores Rider January 27, 2026
so i just found out my thyroid med was made in a factory that got shut down last year… but the label still says FDA approved?? 😭 i feel so betrayed. like… why do they even let us trust anything anymore??
venkatesh karumanchi January 28, 2026
Generics saved my father’s life. He couldn’t afford the brand. He took the generic for 12 years - no issues, no side effects. I’ve seen the results. Don’t let fear silence the truth: for millions, generics are the only way to live.
Kevin Waters January 29, 2026
Both sides have valid points. The system isn’t perfect, but it’s the best we have. The FDA’s 3,500 annual inspections and the 89% patient satisfaction rate show that, for most people, generics work. For narrow-index drugs, work with your doctor. Don’t throw out the baby with the bathwater.
Shelby Marcel January 29, 2026
wait so if the color changes but the medicine is the same… why do i feel weird when i switch? like… is it the dye?? or is it just me??
blackbelt security January 30, 2026
Trust the process. The FDA doesn’t sleep. Every batch is tracked. Every lot is logged. If you’re worried, check the NDC code on the bottle - you can look up the inspection history yourself. Knowledge is armor.
Patrick Gornik January 31, 2026
Let’s deconstruct the myth of equivalence. The FDA’s 80–125% bioequivalence window is a statistical mirage - a neoliberal construct designed to commodify health. The active ingredient may be identical, but the pharmacodynamic signature - the soul of the molecule in the body - is irreducibly unique. We’ve reduced healing to a spreadsheet, and now we’re surprised when people feel… disconnected? When your pill is a barcode, not a cure, you’ve lost more than money - you’ve lost trust in the body’s wisdom. The real scandal isn’t the manufacturing - it’s the epistemology of reductionism.