Endometriosis Treatment: What Works, What Doesn't, and What to Ask Your Doctor
When you have endometriosis, a condition where tissue similar to the uterine lining grows outside the uterus, causing pain, inflammation, and often infertility. Also known as endo, it doesn’t just cause cramps—it can wreck your daily life, relationships, and mental health. Millions of people live with it, yet many are told their pain is "normal" or just stress. The truth? Endometriosis is real, measurable, and treatable—but only if you know what options actually work.
Most treatment plans start with hormonal therapy, drugs that suppress estrogen to slow the growth of endometrial tissue. That includes birth control pills, IUDs like Mirena, or GnRH agonists like Lupron. But these aren’t magic bullets. They can help reduce bleeding and pain for some, but they don’t remove existing scar tissue—and they often come with side effects like mood swings, weight gain, or bone loss. And if you’re trying to get pregnant? Many of these drugs shut down ovulation completely.
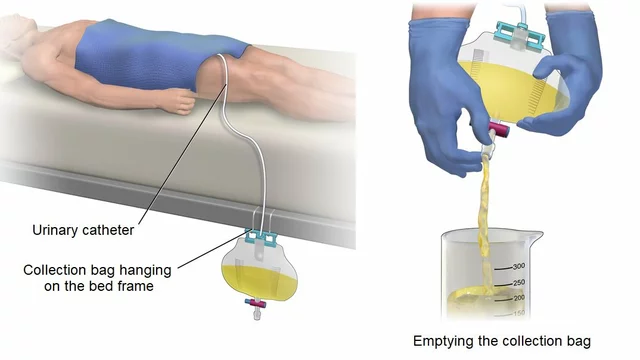
Then there’s laparoscopic surgery, a minimally invasive procedure where surgeons cut out or burn off endometrial lesions. This is the only treatment that physically removes the disease. Studies show it can significantly improve pain and fertility—but it’s not a cure. The tissue often comes back, especially if hormones aren’t managed afterward. And not all surgeons are trained to do it well. A bad surgery can make things worse.
Don’t overlook pain management, a broad category that includes NSAIDs, nerve blocks, physical therapy, and even mindfulness techniques. Many people with endometriosis don’t realize their pain isn’t just from the lesions—it’s from chronic inflammation, muscle tension, and nervous system sensitization. Physical therapists who specialize in pelvic floor dysfunction can help release tight muscles that mimic endometriosis pain. And yes, meditation and breathing exercises aren’t just "nice to have"—they’re backed by research for reducing pain perception.
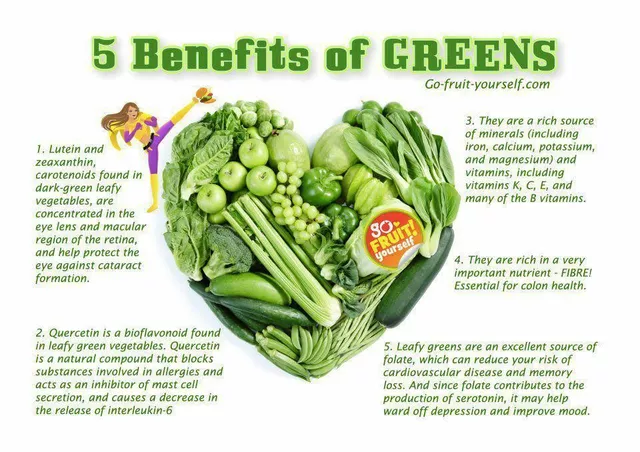
There’s also a growing group of patients turning to diet changes, acupuncture, or supplements like omega-3s and NAC. These aren’t replacements for medical care, but they can help reduce inflammation and support your body’s healing. Just be careful: some herbal supplements interact with hormonal drugs or blood thinners. Always check with your doctor before adding anything new.
What’s missing from most treatment plans? Personalization. Your endometriosis isn’t the same as your friend’s. Stage 1 isn’t always mild. Stage 4 isn’t always the worst. Pain levels don’t match lesion size. That’s why cookie-cutter advice fails. You need a team that listens—gynecologists who specialize in endometriosis, pain specialists, nutritionists, and mental health pros if you need them.
Below, you’ll find real, no-fluff guides on the drugs, procedures, and lifestyle changes that actually help people with endometriosis. No hype. No marketing. Just what works, what doesn’t, and what to ask before you sign anything.
How Atorvastatin May Help Treat Endometriosis: What the Science Says
Atorvastatin, a common cholesterol drug, may reduce endometriosis pain and lesion growth by targeting inflammation. Early studies show promise, but it's not yet a standard treatment. Learn how it works and who might benefit.