How to Prevent Hypoglycemia: Practical Tips for Stable Blood Sugar
When your blood sugar drops too low, you don’t just feel shaky—you can become confused, sweaty, dizzy, or even pass out. This is hypoglycemia, a condition where blood glucose falls below 70 mg/dL, often triggered by diabetes medications, skipped meals, or excessive exercise. Also known as low blood sugar, it’s not just a nuisance—it’s a medical emergency if ignored. If you take insulin or certain oral diabetes drugs like sulfonylureas, you’re at higher risk. But you don’t have to live in fear. Preventing hypoglycemia isn’t about perfection—it’s about awareness, routine, and knowing what to do before it hits.
One of the biggest causes? insulin safety, mistakes in dosing, timing, or matching food intake. Many people take their insulin without checking their blood sugar first, or they skip meals after injecting. Others overcorrect a high with too much insulin, then crash hours later. The fix? Always match your dose to your carb intake and activity level. Use a blood sugar monitoring, a simple, daily practice that gives you real-time feedback. Also known as glucose testing, it’s the single most effective tool to catch a drop before it becomes dangerous.
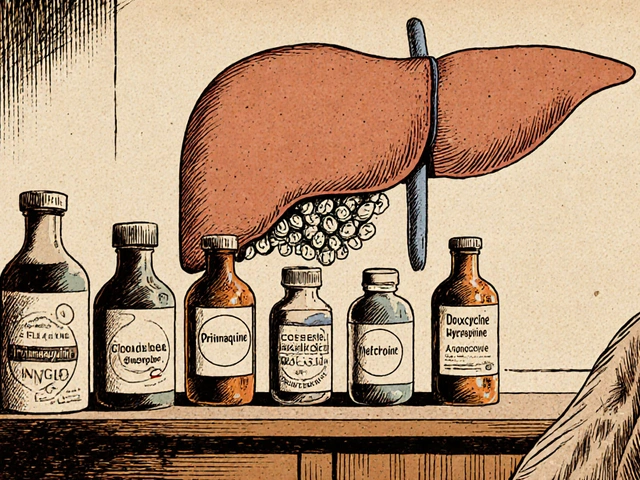
Another hidden trigger? diabetes medications, especially when combined or changed without medical guidance. Some newer drugs like SGLT2 inhibitors lower blood sugar differently than older ones, and mixing them can increase risk. Even switching from brand to generic versions of the same drug can throw off your balance—because inactive ingredients affect how fast your body absorbs the medicine. That’s why talking to your doctor before any switch matters. Don’t assume generics are identical in effect. Your body might react differently, and that’s how hypoglycemia sneaks up.
What you eat matters just as much as what you take. Eating small, balanced meals every 3–4 hours keeps your sugar steady. Carry fast-acting carbs—glucose tablets, juice, or candy—everywhere. Don’t wait until you feel bad to act. If your hands are trembling or your heart is racing, test your sugar. If it’s under 70, eat 15 grams of carbs, wait 15 minutes, then test again. Repeat if needed. This isn’t guesswork—it’s a protocol. And if you live alone or drive, tell someone how to help you if you can’t speak. A medical ID bracelet can save your life.
Exercise lowers blood sugar—great for health, risky if unprepared. Check your levels before, during (if you’re active for over an hour), and after. You might need a snack before working out, or less insulin that day. Alcohol? It blocks your liver from releasing glucose. Even one drink can cause a drop hours later, especially at night. That’s why many people wake up shaky or confused—hypoglycemia while sleeping is silent and deadly.
What you’ll find below are real, tested strategies from people who’ve been there. Posts cover how to read your meds safely, why insulin timing can make or break your day, what to do when generic drugs don’t feel the same, and how to talk to your doctor about avoiding dangerous drops. No fluff. Just what works.
Diabetes and Exercise: How to Prevent Low Blood Sugar During Workouts
Learn how to prevent low blood sugar during exercise with diabetes. Discover proven strategies for carb timing, insulin adjustments, workout order, and tech tools to stay safe and active.