Insulin Therapy: What It Is, How It Works, and What You Need to Know
When your body can’t make enough insulin therapy, a medical treatment that replaces or supplements the body’s natural insulin to regulate blood sugar. Also known as insulin replacement, it’s not just for people with type 1 diabetes—it’s a lifeline for many with type 2 diabetes who’ve run out of other options. Insulin isn’t a cure, but it’s the most direct way to keep blood sugar from going too high or crashing too low. Without it, your cells starve even when there’s sugar in your blood.
Insulin therapy isn’t one-size-fits-all. Some people use long-acting insulin once a day to keep baseline levels steady. Others mix fast-acting insulin before meals to handle spikes from food. There are pens, pumps, and even inhaled versions now. What matters isn’t the delivery method—it’s whether your dose matches your body’s needs. Many people on insulin also track carbs, check blood sugar several times a day, and adjust based on activity, stress, or illness. It’s not just taking a shot; it’s managing a daily rhythm.
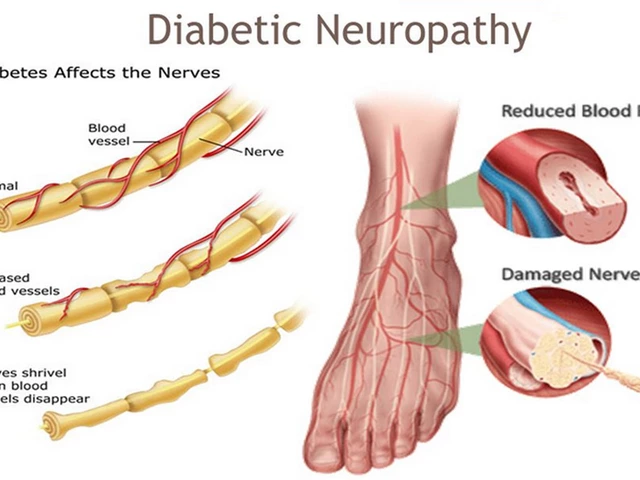
People often assume insulin means failure, but that’s not true. Type 2 diabetes gets worse over time, and your pancreas slowly loses its ability to produce insulin. Waiting too long to start insulin therapy can damage your kidneys, nerves, and eyes. Starting early doesn’t mean you’ve lost control—it means you’re taking charge. And for those with type 1 diabetes, insulin isn’t optional. It’s survival.
Insulin therapy doesn’t happen in a vacuum. It connects to other parts of your health. If you’re on blood thinners, certain supplements like ginkgo biloba can increase bleeding risk when combined with insulin. If you’re managing heart disease or kidney issues, your insulin dose may need tweaks. Even something as simple as a change in your sleep schedule can throw off your blood sugar. That’s why smart pill dispensers help some people stay on track—not just with insulin, but with all their meds.
You’ll also see insulin mentioned alongside other diabetes drugs like metformin, empagliflozin, or GLP-1 agonists. These aren’t replacements for insulin—they’re often used together. Metformin helps your body use insulin better. SGLT2 inhibitors like empagliflozin help your kidneys flush out extra sugar. But when those aren’t enough, insulin steps in. It’s the final tool in the toolbox, and sometimes the most powerful one.
There’s a lot of fear around insulin: weight gain, needles, low blood sugar. But most of that fear comes from outdated stories. Modern insulins are cleaner, more predictable, and easier to use. And yes, you can still live a full life—travel, work, exercise, eat out—while on insulin therapy. It just takes learning the rules of the game.
Below, you’ll find real-world guides on managing medications, understanding drug interactions, and making sense of your treatment plan. Whether you’re new to insulin or have been on it for years, these posts give you practical ways to stay safe, avoid mistakes, and take back control.
Type 1 Diabetes: Symptoms, Diagnosis, and Insulin Therapy Options
Type 1 diabetes is a lifelong autoimmune condition requiring insulin therapy. Learn the key symptoms, diagnostic tests including autoantibodies and C-peptide, and modern insulin delivery options like pumps and CGMs. Understand targets, daily management demands, and new advances like teplizumab and stem cell therapy.